Insulin Uses and Side Effects-Know It All
Table of Content
- What is Pancreas?
- Why is insulin needed in the body
- Role of insulin in the body
- What is diabetes type I, II and Gestational diabetes?
- Curing Diabetes with Insulin
- How is insulin manufactured?
- How to administer insulin
- Uses of Insulin
- Drawbacks of using insulin
- Side effects of using Insulin
- How to avoid side effects
- Lifestyle modifications while using insulin
- Long-term drawbacks of insulin
- Living a healthy life while on insulin
What is insulin?
Insulin is a hormone produced by the pancreas that is involved in maintaining the balance of glucose in body. Insulin doesn’t do this job alone, hormone glucagon which too is a pancreatic hormone helps maintain the balance of glucose in our body. Here we will know everything about the uses and side effects of insulin.
What is Pancreas?
Pancreas is a glandular organ found in the abdomen which is a part of the digestive system. It is important for digesting food and regulating blood glucose levels. The portion of the pancreas which is responsible for producing digestive enzymes is called the exocrine portion and the other portion that secretes hormone is called endocrine portion. The endocrine portion of pancreas contains two types of cells, namely alpha cells that are responsible for producing the hormone glucagon and the beta cells that are responsible for producing the hormone insulin. The action of glucagon is to stimulates the liver for producing glucose from glycogen when there is decreased blood glucose levels. Whereas, insulin promotes reduction in blood glucose levels by stimulating the liver to store glucose in the form of glycogen.
Insulin reduces blood sugar level while Glucagon increases blood sugar level.
Why is insulin needed in the body?
Insulin is a hormone that is required by the cells in order to remove glucose from the blood and use it to produce energy. Cells require glucose to produce energy to carry out their function.
Some facts about insulin
- In 1922, researchers gave an active extract of active pancreas containing insulin to a patient whose body did not regulate the blood glucose levels.
- Purified animal-sourced insulin was the only type of insulin available to diabetics until genetic advances occurred later with medical research.
- First commercial insulin was approved by the U.S. FDA in 1939 which was actually purified form of animal insulin.
- First synthetic insulin was produced simultaneously in the early 1960s
- The first synthesis of crystalline bovine insulin with biological activity was achieved by Chinese researchers in 1965.
- The first genetically engineered, synthetic “human” insulin was produced using E. coli in 1978.
- The first recombinant insulin was approved by the U.S. FDA in 1982.
- In 1982 the first commercially available biosynthetic human insulin was sold under the brand name Humulin
- Currently, the insulin that is used for treating patients with diabetes is either from animal sources (bovine or porcine) or human analogue insulin that is produced through recombinant DNA technology.
- The vast majority of insulin currently used worldwide is biosynthetic recombinant “human” insulin or its profile.
- Synthetic insulin can trigger adverse effects, so some people with diabetes rely on animal-source insulin
- Insulin is usually taken as subcutaneous injections by single-use syringes with needles, insulin pump, or by insulin pens with disposable needles.
- Inhaled insulin is also available in the U.S. market now.
- Unlike many medicines, insulin currently cannot be taken orally because, it gets broken down in stomach and loses all its activity.
Role of Insulin in the Body:
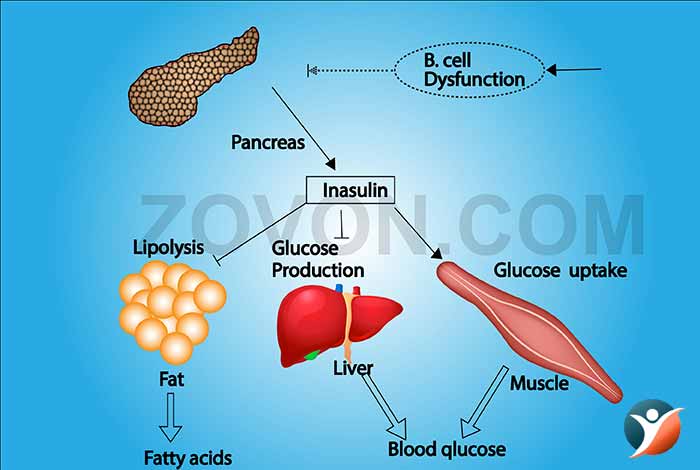
The main role of insulin is the regulation of blood glucose levels in the body. When there is a lack of insulin in the body or the cells do not respond to it, it can lead to diabetes the disease we all are familiar with.
Apart from its role in regulating blood glucose levels in the body, insulin also plays a role in storing fat in the body. Insulin determines how glucose and fat are used and stored in the body.
Insulin signals the liver, muscles and fat cells to take up glucose from the blood and utilize it to carry out different life processes. If there is enough energy in the body, insulin then signals the liver to take up the excess glucose and store it in the form of glycogen.
The liver has a capacity of storing nearly 5% of its mass in the form of glycogen.
Some cells of the body are able to take up glucose from the body without using insulin, but most of the cells require insulin to facilitate uptake of glucose.
What is diabetes?
Diabetes is a condition in which the blood glucose levels, also known as blood sugar level, becomes elevated. Blood glucose is the main source of energy in the body and is obtained from the food that we consume. Sometimes, the body does not make any insulin or the cells develop resistance to the hormone and the cells are not able to take up glucose from the blood. This causes the glucose levels to spike up. This condition is referred to as diabetes.
Over time, excessive blood glucose in the body starts causing health issues like damage to kidneys and eyes.
Although there is no cure for diabetes, but this disease can be successfully managed with medication and modifications in diet and lifestyle. Diabetes is a bunch of disorders are can be of following types:
1. Type I Diabetes
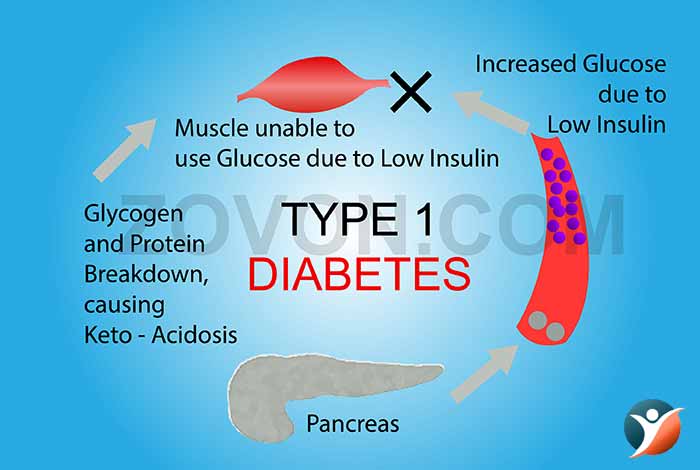
Type I diabetes occurs when the beta cells of pancreas do not produce enough insulin. The immune system attacks and destroys pancreatic cells synthesizing insulin. This form of diabetes is generally diagnosed in children and young adults. Sometimes, even adults can be diagnosed with type I diabetes.
2. Type II Diabetes
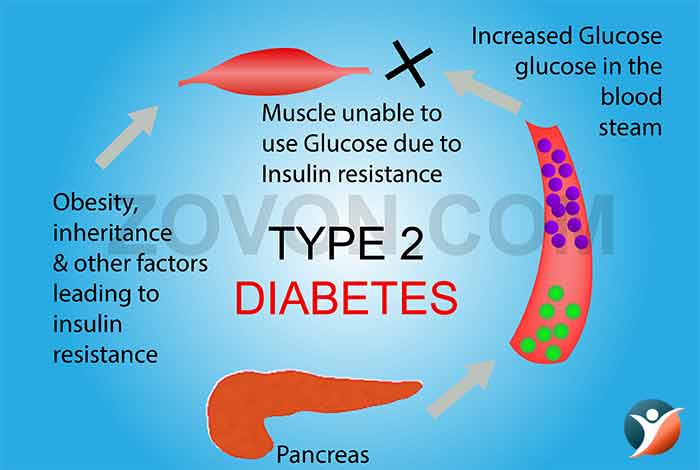
A person suffering from type II diabetes develops resistance against insulin. This disease can develop in people at any age, but is most common in people of the middle age and older people. It is the most common type of diabetes.
3. Gestational Diabetes
Gestational diabetes sometimes develops in pregnant women, which generally goes away after the birth of the baby. However, it is seen that these women generally develop type II diabetes later in life. In the recent times, some other types of diabetes have been identified as well. These are;
4. Type 1.5 Diabetes
Type 1.5 diabetes is an unofficial term that is used for referring to a form of type I diabetes known as Latent Autoimmune Diabetes in Adults (LADA). The term 1.5 is used because this form of type I diabetes shares some of the features of type II diabetes. This type of diabetes develops in adulthood and has a slow onset of action, similar to type II diabetes but it is also an autoimmune disease just like type I diabetes.
This type of disease is most often misdiagnosed as type II diabetes.
5. Type 3 Diabetes
Type 3 diabetes is the term allocated to diabetes arising due to development of insulin resistance in the brain, causing Alzheimer’s disease. Researchers at the Warren Alpert Medical School at Brown University have raised the possibility of development of insulin resistance in the brain as a reason for progression of Alzheimer’s disease. As per a study carried out in 2012 by the scientists at the University of Pennsylvania indicated that Alzheimer’s disease can develop in the absence of significant hyperglycemia in the brain.
6. Type 3c Diabetes
Diabetes type 3c is a misdiagnosed form of diabetes type II. Whenever diabetes arises due to diseases of pancreas, it is called diabetes type 3c. Some of the diseases that can cause diabetes type 3c include pancreatic cancer, cystic fibrosis, chronic pancreatitis or resection of pancreas. In these conditions, there is inadequate production of digestive enzymes by the exocrine portion of the pancreas which leads to improper control of blood glucose levels.
7. Type 4 Diabetes
Scientists at the Salk Institute labs of Ronald Evans and Ye Zheng discovered type 4 diabetes that was found to occur in lean elderly people. This type of diabetes was found to occur due to old age. Genetics or obesity were not found to be the reasons for this type of diabetes.
8. MODY
MODY refers to maturity onset diabetes of the young. This type of diabetes arises due to mutations in the gene present on chromosome 2 and is responsible for the transcription of neurogenic differentiation 1 factor. This factor promotes the transcription of genes responsible for producing insulin, formation of beta cells of pancreas and parts of nervous system. Only 3 kindreds have been identified till date with this rare mutation. Other members of the family were found to have more typical form of type 2 than these patients. The exact reason behind the difference in expression of these genes have not been identified. Most of the members of the family were diagnosed with diabetes after the age of 40 years and only some people required insulin to manage their blood glucose levels.
9. Neonatal Diabetes mellitus (NDM)
Neonatal diabetes mellitus refers to a type of diabetes that affects infants in the age of 6- 12 months. It is a rare condition in which the body does not produce enough insulin, causing an increase in blood glucose levels. It is often mistaken for type I diabetes.
However, type I diabetes is not observed in the first 6 months of life. Any diabetes that manifests itself in the first 6 months of life is bound to have genetic reasons.
Scientists have identified a number of genes and mutations that might result in NDM. In almost half of these babies, the condition lasts for a lifetime and is then called Permanent neonatal diabetes mellitus (PNDM). In the rest of the patients in which the diabetic condition is transient and disappears during infancy but can reappear later in life is called transient neonatal diabetes mellitus (TNDM).
The symptoms observed in this condition depend on the type of mutation and the gene affected.
10. Cystic Fibrosis Related Diabetes (CFRD)
People with cystic fibrosis develop a unique type of diabetes which shares some of the features with type I and some with type II diabetes. In people with cystic fibrosis, the characteristic sticky mucus is responsible for damaging the pancreatic cells responsible for making insulin. This causes the body to produce insufficient amounts of insulin in the body. The body does not respond properly to insulin that is produced, especially at the time of illness, while on steroids and when pregnant. This state is referred to as insulin resistant.
The most dangerous thing about CFRD is that patient is unaware of its diabetic state unless tested.
Curing Diabetes with Insulin
Insulin therapy is incorporated in the treatment plan of diabetes in different ways, depending on the type.
1. Insulin and Type I Diabetes
In people suffering from type I diabetes, the body produces insignificant amounts of insulin to regulate blood glucose levels in the body. In the absence of insulin, the blood glucose levels spike and can have serious consequences. People with type I diabetes are required to go on an insulin therapy as soon as the diagnosis is made.
2. Insulin and Type II Diabetes
Type II diabetes develops when the body is not responding to insulin that is being produced by the pancreas. This state is called insulin resistance. In the later stages of the disease, the extra demand of the body to keep blood glucose levels in check can lead to loss of insulin producing cells in the pancreas. Therefore, depending on the level of insulin resistance present in the body, people might be required to take insulin therapy in order to get their blood glucose levels in control.
Otherwise, in the early stages of the disease, anti-diabetic drugs are enough to manage the blood glucose levels.
3. Insulin and CFRD
CFRD can be easily managed through insulin therapy while monitoring the blood glucose levels, consuming high calorie diet and staying physically active. It is important for people with CFRD to consume high calorie, high fat, high protein and high salt diet in order to achieve and maintain a healthy weight and nutritional status. Since carbohydrates get converted into glucose in the blood, it is important for people with CFRD to count the calories before eating so as not to increase their blood glucose levels too high. Calorie counting also helps patients to determine the exact dose of insulin required to keep blood glucose levels in check.[1]
4. Insulin and Type 1.5 Diabetes
People who are diagnosed with type 1.5 diabetes eventually depend on insulin for treatment and might be required to start the therapy within months or years of diagnosis.
This is in contrast to people with type 1 diabetes who are required to start the therapy within a few weeks of diagnosis.[2]
5. Insulin and Neonatal Diabetes Mellitus
In most of the cases of neonatal diabetes mellitus, the infant is treated with oral hypoglycemics. Genetic tests are done to determine whether the child will require insulin therapy.
6. Insulin and Type 4 Diabetes
The treatment of type 4 diabetes is currently focused at blocking T regs from getting accumulated in the body and therefore, insulin is not found to play any role in the treatment regime of the disease.
7. Insulin and Type 3 Diabetes
The treatment of type 3 diabetes has not been finalized yet and at present it is being treated with the help of medicines. More studies are required to fully understand the principles of diagnosis and treatment of type 3 diabetes.
8. Insulin and Type 3c Diabetes
Insulin should be included in the treatment plan of diabetes type 3c. However, due to misdiagnoses, the insulin therapy is often missed which can cause serious complications.
9. Insulin and Gestational Diabetes
When gestational diabetes cannot be managed through lifestyle changes or medicines, then insulin therapy is recommended as the last resort for keeping blood glucose levels in check.
How is insulin manufactured?
Human insulin is manufactured in the lab using a bacteria Escherichia coli (E. coli) and sometimes yeast (Saccharomyces cerevisiae) with the help of DNA recombination technology. This is a genetic engineering process in which the genetic material of the bacteria is modified so that it can produce human insulin. The primary insulin molecule produced by the bacteria is then processed to finally obtain human insulin.
Before recombinant DNA technology became popular, animal insulin obtained from cows and pigs. It was the first type of insulin that was used for managing the symptoms of type I diabetes. Animal insulin is taken from the pancreas of the animals, purified and packaged for sale. The animal insulin is purified in order to reduce the chances of development of adverse reaction to it.
How to administer insulin
An insulin regimen is developed in order to manage the symptoms of insulin dependent diabetes. In all cases, the insulin dose is tailormade for the patient, depending on the type of disease and the amount of insulin produced naturally in the body. It also needs to be balanced with a healthy diet and regular exercise.
1. Mixing Insulin
Sometimes, the patient is required to mix rapid or short acting insulin with intermediate or long acting insulin in order to produce normal levels of glucose in the body. Mixed insulin is known to give better results than single insulin. However, mixing of insulin should only be done if it is suggested by the doctor. There are a number of facts that need to be considered before mixing two different types of insulin like particle aggregation, absorption rate, bioavailability and so on. Consultation with doctor is therefore extremely necessary before mixing.
2. Syringes
The administration of insulin requires subcutaneous injection of insulin using syringes that are marked in insulin units. The making on the insulin syringes can vary depending on the manufacturer. Also, these syringes are available in different lengths.
In the recent times, a number of different medical devices have been developed in order to reduce the risk of needle sticks and other injuries as per the OSHA standards. These devices have a special feature to prevent needle injuries. These may come with engineered sharps injury protection (ESIP) feature that helps in reducing the injuries. Patients should make sure that they should never share their syringes with other people.
3. Disposal
Recapping, breaking or bending the needle increases the chances of getting needle-stick injury. Insulin pens, syringes, needles and lancets should be disposed off as per the local guidelines. Some areas might have a special needle disposal program in place that prevents the mixing of sharp objects with the regular waste.
4. Needle Reuse
Manufacturers discourage reusing the needles that are meant for single use due to the concern for sterility. Reusing needles might also increase the chances of spread of infections for some patients. Another concern is the needle tip becoming bent after use. If such a needle is used for administering insulin again, there are chances of injuries.
If needle reuse is being considered by the patient, he should make sure that he is capable of maintaining the required sterility and safety. Reused syringe should be kept at room temperature. The risks or benefits of refrigerating needles is not properly understood. Wiping needle surface with alcohol is not desired as it might erode the silicon coating of the needle that might make skin puncture a more painful experience.
5. Syringe Alternatives
There are a number of syringe alternatives available in the market like jet injectors, pens and insulin delivery aids like non-visual insulin measurement devices, vial stabilizers, needle guides and syringe magnifiers.
Jet injectors give out a fine stream of insulin into the skin and is the option that is best for people who have syringe phobia or are unable to use syringes. Several pen-like devices and insulin containing cartridges are available in the market that can deliver insulin subcutaneously.
6. Dose Preparation
Before each injection, the label at the insulin bottle should be verified in order to avoid injecting an incorrect dose of insulin. The injection site and hands should be clean. The vial or pen should be gently rubbed between the palms of the hands in order to re-suspend the insulin. After drawing insulin into the syringe, the fluid should be checked for air bubbles. Air bubbles are not dangerous in themselves but can decrease the injected dose.
7. Injection Procedures
Injections are given in the subcutaneous tissue. Lightly grasp a fold of skin, release the pinch and inject at an angle of 90 degrees. Children and thin individuals might use short needles or need to pinch the skin and then inject at 45 degrees in order to avoid intramuscular injection, especially in the thigh area.
8. Injection Site
Insulin should be injected in the subcutaneous tissue of the upper arm and the anterior and lateral portions of the thigh, abdomen and buttocks. Intramuscular injection is not recommended for routine delivery of insulin. It is important to rotate the injection site in order to prevent lipohypertrophy or lipoatrophy. It is recommended to rotate within one area rather than moving to a different area with each injection. This practice reduces the variation of absorption on a day to day basis. [3]
Uses of Insulin
Apart from maintaining normal blood glucose levels, insulin is known to posses the following additional properties:
- Wound healing
- Parenteral Nutrition
- Anti-aging
- Body building
- Weight management
- Therapy for poisoning
- Insulin induced hypoglycemic treatment
- Metabolic oncolytic treatment regimen
- Breast augmentation [4]
Drawbacks of using insulin
The biggest drawback of using insulin therapy is the chance of developing low blood sugar levels in the body if too much of insulin is administered. Other drawbacks are associated with the mode of delivery of insulin like needle injuries. Weight gain is also observed by many patients. Insulin therapy is not economical as well and in the recent times, there has been an upsurge in the prices of insulin that is making it impossible for the patients to continue this therapy.
Side effects of using Insulin
Some of the commonly observed side effects of insulin therapy are as follows:
- Hypoglycemia, in which the blood glucose level becomes too low
- Weakness
- Blurry vision
- Weight gain
- Sweating
- Tremors
- Irritability
- Rapid breathing
- Fast Heart rate
- Fainting
- Seizure
Other side effects include redness, pain, itching or thickening of skin at the site of injection. These side effects usually go away in few days. A recent study has even indicated that taking insulin for treating type II diabetes can make the person more susceptible to many serious health conditions like stroke, heart attack, eye complications and cancer.[5]
If any other side effects are being observed by the patient, it should be reported to the doctor without any delay.
How to avoid side effects
There are a few ways by which the side effects of insulin therapy can be avoided. These are as follows:
- Informing doctor about any allergic reaction related to insulin therapy
- Informing the doctor about all prescription and non prescription medicines that are being taken
- Avoiding or reducing alcohol consumption
- Informing doctor about any kind of nerve damage that has occurred due to diabetes
- Planning of pregnancy should be under medical supervision
- Understanding what measures are to be taken in case of hypoglycemia
- Telling your family, friends, care givers, teachers and guardians about how to manage an emergency situation arising due to hypoglycemia
- Getting blood glucose levels tested on a regular basis
Life style modifications while using insulin
In order to make sure your insulin therapy work successfully, the patients should make the following changes in their lifestyles:
- Measuring blood glucose levels regularly
- Consuming a diabetes-friendly diet
- Sticking to insulin schedule religiously
- Staying hydrated
- Exercising regularly
- Being prepared every time for an emergency arising due to hypoglycemia
- Smoking cessation
- Managing stress effectively through stress management techniques like yoga and
- Pilates
- Reducing consumption of alcohol [6]
Long term drawbacks of insulin
Some of the long-term drawbacks of insulin include the following effects:
- Hypoglycemia
- Cold sweats
- Palpitations
- Allergic reactions
- Skin thickening at the site of injection
Living healthy life while on insulin
It is possible to lead a healthy life while being on insulin therapy. All it requires is a healthy lifestyle with regular exercise and monitoring of blood glucose levels. An insulin injection should not stop the pace of your life.