
Overview and Statistical Facts of Sleep Apnea
Apnea is a Greek word, which means “without breathing.” Sleep Apnea is a severe sleeping disorder, which is marked by interruptions in breathing during sleep. These interruptions are brief, lasting for few seconds and occur several times, while a person is asleep. A loud snore and a feeling of tiredness even after sleeping for adequate hours, are the usual signs of sleep apnea.
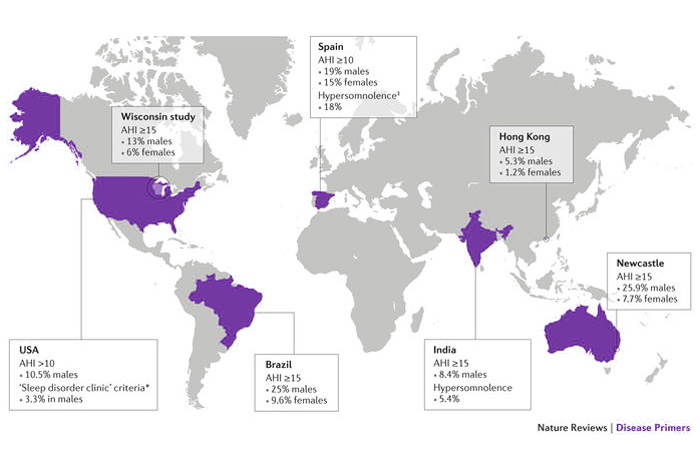
As per an estimate by the National Sleep Foundation, sleep apnea affects more than 18 million American adults, with males being more commonly affected by this condition than females. It is not uncommon in children too, affecting almost 2 to 3% of children in America.
Sleep apnea is caused by an obstruction of the airway and/or by a failure of brain to send signals to the muscles of breathing. In either case, sleep apnea can severely deteriorate the quality of life of an individual. Being obese, smoking, excess consumption of alcohol, flu, nasal congestion and several other factors put a person at a higher risk of developing sleep apnea.
The transient lapse in breathing during sleep can hamper the flow of oxygen to brain and rest of the body, causing several complications in the long run. A disturbed sleep can dramatically affect mental performance, energy and long-term health of an individual.
But, sleep apnea is an absolutely treatable condition. It can usually be treated with the aid of air pressure devices, oral appliances and surgery (in severe cases). However, if left untreated, sleep apnea can be a life-threatening condition.
Types of Sleep Apnea
There are two major types of sleep apnea, which are described below.
Obstructive Sleep Apnea or OSA
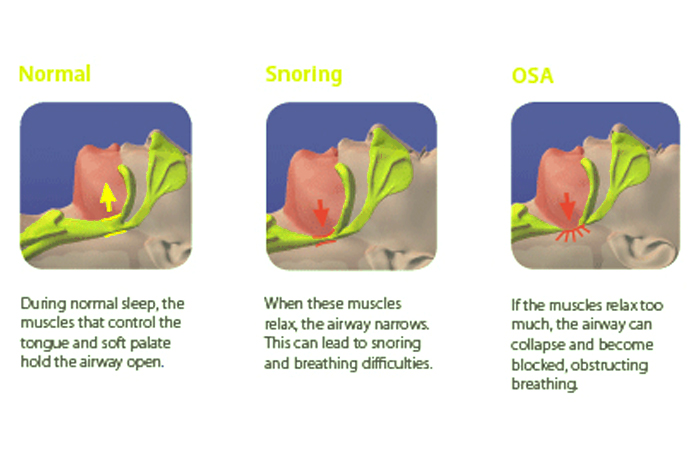
- It is the most common form of sleep apnea and occurs due to a blocked airway. The blockage is caused by the relaxation of the soft tissue present at the back of the throat.
Central Sleep Apnea
- It is caused due to brain’s inability to command the muscles to breathe. This happens because of the respiratory control center’s instability. Central sleep apnea has nothing to do with the airway.
A third type of apnea exists, which is a combination of both, obstructive and central sleep apnea. This variant is known as complex sleep apnea syndrome or treatment-emergent central sleep apnea.
Symptoms of Sleep Apnea
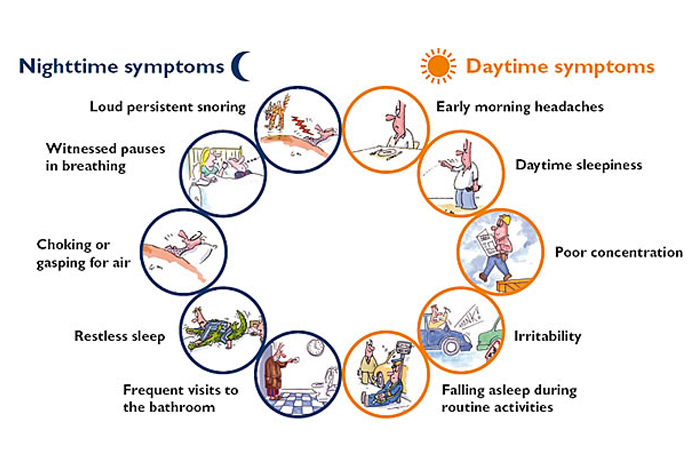
Obstructive and Central sleep apnea produce similar symptoms, often posing difficulty in accurate diagnosis. These symptoms are as follows.
- Loud Snoring (generally in the case of OSA)
- Discontinuous breathing pattern (observed by someone else)
- Waking up with a sore throat or dry mouth
- Partial awakenings caused by breath shortness (generally in the case of central sleep apnea)
- Morning headache
- Irritability and concentration related issues
- Insomnia, i.e., inability to sleep
- Hypersomnia (sleepiness during the daytime)
- Chest pain or sweating while sleeping
- Mood changes, forgetfulness and a reduced sex drive
Risk Factors of Sleep Apnea
Sleep apnea can affect people of all age and gender. However, presence of certain factors put a person at a higher risk of developing sleep apnea. These factors are as follows.
Gender
Males are twice more prone to develop sleep apnea. However, overweight and post-menopausal women are also at a high risk of developing sleep apnea.
Age
Chances of sleep apnea increase with age and is more common after the age of 40.
Ethnicity
People of certain ethnic origins namely, African-Americans, Hispanics and Pacific-Islanders, are at a higher risk of developing sleep apnea.
Overweight
Excess weight increases the risk of developing sleep apnea to four-folds. The extra fat around the upper airway obstructs the breathing while sleeping and causes sleep apnea. However, not everyone who has sleep apnea is overweight.
Circumference of Neck
Having thicker necks can narrow down the airway. Neck circumference more than 17 inches or more in men and 16 or more inches in women increases the risk of developing sleep apnea.
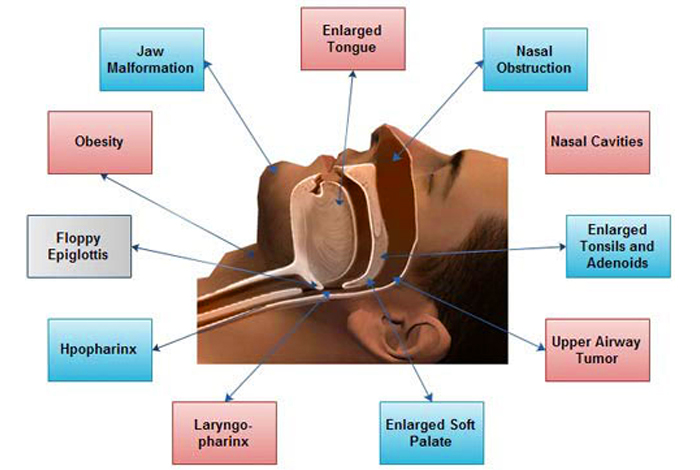
Conditions causing narrowing of airway
Some people may have inherited a narrow airway. Such people are at a greater risk of developing sleep apnea. Also, having a large tongue, large tonsils, a small jaw and enlarged adenoids, can also lead to a narrow airway and cause sleep apnea.
Nasal congestion
Any nasal obstruction caused by sinus inflammation, allergies or an anatomical defect, like Deviated Nasal Septum (DNS), increases the risk of developing sleep apnea.
Family History
Sleep apnea runs in family. So, if you have parent or sibling suffering from sleep apnea, you are at a high risk of developing it too.
Alcohol, Sedatives and Tranquilizers
These agents act as potent relaxants and relax the soft tissues at the back of the throat. Alcohol may also alter the control of brain on the muscles responsible for breathing, thus causing apnea. Hence, these factors act as significant risk factors for the development of sleep apnea.
Smoking
Smokers are three times more prone to develop sleep apnea. Smoking causes fluid retention and inflammation in the upper airway, causing difficulty in breathing and sleep apnea.
Heart diseases
People suffering from congestive heart failure, are at a higher risk of developing sleep apnea.
Stroke
People who have had a stroke are at a greater risk of developing sleep apnea.
Narcotic pain-killers
These medications act on the brain and relieve pain. Hence, people on narcotic pain medications are at a high risk of developing sleep apnea.
Hormonal Imbalances
Certain disorders of hormonal disparity, such as hypothyroidism, PCOS, or imbalances in growth hormone, testosterone, etc. can trigger sleep apnea.
Do I have Sleep Apnea?
Most of the times, a person suffering from sleep apnea is unaware of the breathing difficulty he or she is experiencing at night time. Thus, snoring at night time is usually complained by other family members and is a strong indicator of sleep apnea.
However, if you experience wakefulness several times or gasp for breath at night time, you most probably have sleep apnea. If you are overweight or obese or have a thicker neck, you are at a high risk of developing sleep apnea.
If you wake up with a headache or feel sleepy throughout the day, you are most likely facing breathing distress at night and are suffering from sleep apnea. Irritability, an inability to concentrate and mood changes may also be suggestive of a disturbed sleep and may be due to sleep apnea.

Causes of Sleep Apnea
The cause of sleep apnea varies with the type of sleep apnea. Obstructive sleep apnea is caused by relaxation of muscles present at the back of the throat. The primary function of these muscles is to support various structures of mouth and throat, including soft palate, tongue, uvula (triangular tissue hanging at the back of throat) and tonsils. When the muscles at the back of the throat relax, all these structures thin down the airway, causing difficulty in breathing. This causes you to snore or wake up several times in your sleep to gasping for breath. However, this wakeful period is extremely brief to be remembered by the individual next day.
In contrary, central sleep apnea is not caused due to impaired muscle function. Rather, it occurs when your brain cannot guide your muscles efficiently to contract and relax. This lack of co-ordination can render you short of breath while asleep, leading to sleep apnea.
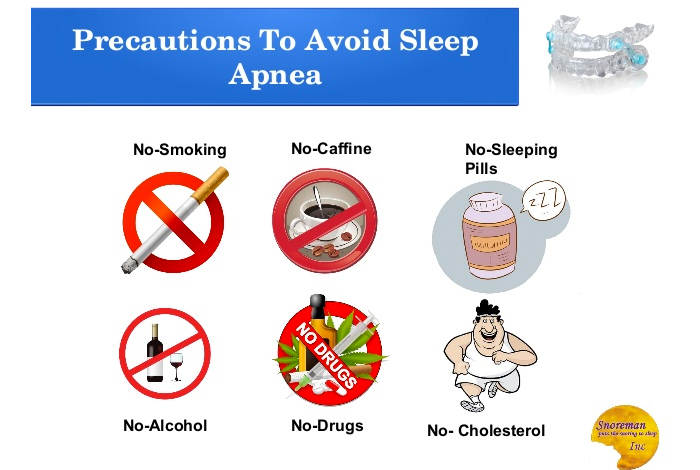
Prevention
Central sleep apnea is caused by brain’s inability to transmit signals to respiratory muscles, hence can’t be prevented. However, OSA can be prevented by following methods.
Maintain a healthy weight
Overweight is a major risk factor of sleep apnea. Hence, maintaining a healthy weight can play a crucial role in preventing sleep apnea. Exercise and a balanced diet can aid in losing the excess weight, thus reducing the risk of developing sleep apnea.
Avoid alcohol and smoking
As already stated, alcohol consumption and smoking increases the risk of developing sleep apnea. Therefore, refrain from alcohol and smoking to prevent sleep apnea.
Talk to your doctor
Certain medications, like sedatives relax the throat muscles, causing sleep apnea. Hence, discuss with your doctor and ask for alternatives.
Diagnosis and Tests of Sleep Apnea
After taking a thorough account of symptoms being experienced by a patient, the physician may refer the patient to a sleep disorder center for an accurate diagnosis. The diagnosis of sleep apnea is done by assessing the breathing pattern and the body functions of a patient while the patient is asleep. This is done by following tests.
Nocturnal Polysomnography
In this test, an equipment is hooked up to the patient, which monitors his lung, heart and brain activity, leg and arms movements and levels of oxygen in blood, while the person is asleep. The tests which aid in assessing these parameters include Electroencephalogram (EEG), Electromyogram (EMG), Electrocardiogram (ECG), nasal airflow sensor, etc.
Home Sleep Tests
Some patients may be advised to do some tests at home. These include measuring the airflow, heart rate, breathing pattern and blood oxygen levels. If the results show a drop-in level at sleep time and higher readings in wakeful state, the person is diagnosed to have sleep apnea.
ENT examination
If the above tests are suggestive of a sleep apnea, your doctor may refer you to an Ear Nose and Throat (ENT) specialist. This is done to rule out any nasal congestion or obstruction, which can cause obstructive sleep apnea.
Neurological Examination
If obstructive sleep apnea is ruled out, the doctor then does a neurological examination to look for brain abnormalities which can cause central sleep apnea.
Ruling out other reasons
Some hormonal imbalances, like hypothyroidism, PCOS, etc., cause sleep apnea. Hence, your doctor may order blood tests to check levels of thyroid hormone, testosterone, growth hormone, etc. A pelvic ultrasound may be ordered as an investigation for PCOS.

Treatment of Sleep Apnea
The treatment of sleep apnea varies according to the degree of severity of the condition. Mild cases of sleep apnea can be treated with lifestyle changes. If examination reveals nasal allergy, your doctor may recommend treatment for allergy. However, if the apnea is moderate to severe, or if the patient is not responding to traditional methods, you may require assistance of certain devices or surgery.
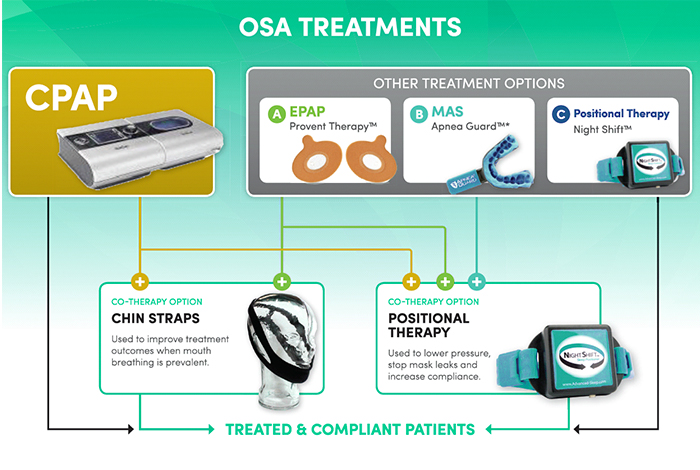
1. Therapies for Obstructive Sleep Apnea
There are various therapies, which can be used for the treatment of obstructive sleep apnea. These are as follows.
Continuous Positive Airway Pressure (CPAP): In CPAP treatment, the patient wears a mask around the mouth or nose during sleep. The mask is connected to a machine that provides a continuous flow of air inside the nose, which helps in keeping the airway open and regulates the breathing cycle. There are different types of masks available, hence a patient may have to try many to get the most-suited one. However, if a patient is struggling with the CPAP, he/she must not discontinue using it. Instead, consult your doctor for modifications. But, if the condition does not improve, or patient experiences any weight changes, other treatment modalities must be tried under the guidance of a physician.
Other Airway Pressure Devices: If CPAP does not seem effective, patient may be advised to use other airway pressure devices, such as Auto- CPAP or bilevel positive airway pressure (BiPAP) device. Auto-CPAP device automatically changes the pressure of airflow while a person is asleep. BiPAP device supplies bilevel positive airway pressure, i.e., it supplies more pressure while inhaling and less pressure while exhaling.
Expiratory Positive Airway Pressure (EPAP): These are small, single-use airway pressure devices, placed on each nostril before going to sleep. This device has a valve, which allows free movement of air while inhaling. When one exhales, air passes through small holes in the valve. This causes an increase in pressure in the airway, keeping it open. However, EPAP is beneficial for people suffering from mild sleep apnea, or those not responding to CPAP.
Oral Appliances: These appliances are meant to keep the throat open during sleep. Some bring the jaw forward, thus relieving snoring and mild cases of obstructive sleep apnea. Although these are less effective than CPAP, they are easier to use.
2. Surgery
It is usually indicated once all other therapies have been tried for at least 3 months. However, if examination reveals structural abnormality in jaw, throat or nose, surgery is advocated as a first line treatment.
The goal of surgery is to enlarge airway, remove blockage (if any) and relieve symptoms of sleep apnea. Various surgical options are as follows.
Tissue Removal (uvulopalatopharyngoplasty): In this procedure, doctor removes tissue from the top of the throat and back of the mouth. This procedure also involves removal of tonsils and adenoids. It is done for patients who can’t tolerate oral appliances and CPAP. The tissues at the back of the throat is removed using radiofrequency energy.
Jaw Repositioning (Maxillomandibular advancement): This procedure involves moving the jaw forward relative to the remaining bones of the face. This enlarges the space behind the soft palate and tongue, thus relieving the breathing difficulty at night.
Creating a new airway (Tracheostomy): In case of severe fatal sleep apnea, surgeons creates an opening in the neck of the patient and insert a plastic or metal tube to aid in breathing.
Nasal surgeries: If doctor suspects a nasal polyp or a deviated nasal septum, a surgery may be performed to correct it.
OTC Medication and Self-Management Methods
Some of the over-the-counter(OTC) medicines that are available for treating sleep apnea include Diphenhydramine hydrochloride and Doxylamine. However, these medicines should only be used when prescribed by a physician.
Moreover, various nasal decongestants like oxymetazoline, pseudoephedrine, phenylephrine are available as over the counter medicines that can be used for the treatment of mild sleep apnea.
Sleep apnea can also be treated with the help of several self-management methods like:
Weight Management
Healthy weight should be maintained in order to manage sleep apnea.
Limiting alcohol and Stopping Smoking
Smoking, alcoholism and abusing sleeping pills should be avoided for treating sleep apnea.
Proper Management of Allergies
Nasal allergies can make it extremely difficult to sleep and breath properly. During an episode of nasal allergy, the tissues of upper throat swell up and make the airway narrow. As the space becomes less, breathing becomes difficult.
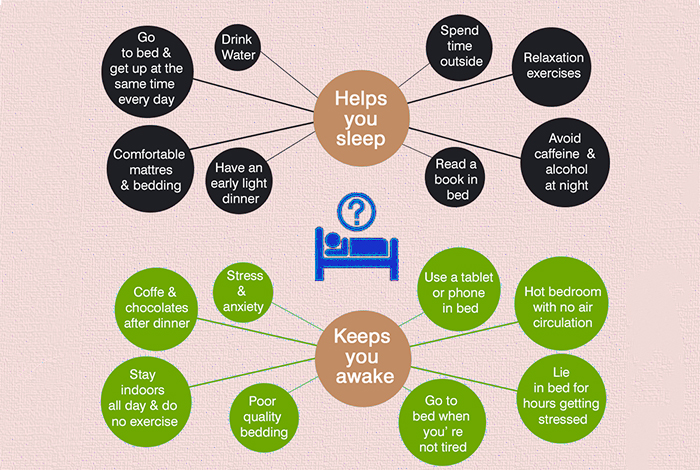
Building a Good Sleep Routine
It is important to maintain a good sleep routine for better health. However, sleep apnea makes it difficult to get proper sleep. Most of the people have troubled breathing when sleeping on their back. therefore, patients must try sleeping in other positions where their breathing is relaxed.
Natural Ways to Cure Sleep Apnea
Despite all the equipment and surgical methods that are available to treat sleep apnea, sometimes patients need to find a cure from the natural resources. Some of the ways by which sleep apnea can be treated naturally include:
- Maintaining a healthy weight by consuming fiber and protein rich diet helps in managing sleep apnea. Foods that are loaded with unhealthy fats should be avoided. Exercises such as HIIT (High-intensity Interval Training) when included in the daily routine can help in managing the condition.
- Stopping smoking, alcohol consumption, or taking sleeping pills can help in the treatment of sleep apnea. These factors are known to cause inflammation in the airway resulting in breathing problems while sleeping.
- Treating various other conditions like nasal congestion, coughs and acid reflux can be helpful in treating sleep apnea naturally.
- Humidifying the bedroom can be helpful in effective and natural management of sleep apnea.
- Trying a different sleeping position and maintaining proper sleep hygiene can also be helpful in reducing the symptoms of sleep apnea without any medication.

Health Tip by Experts
Sleep apnea is a serious sleep disorder that affects not only your sleep, but the sleep of our family members as well. So, get yourself treated, sleep and let others sleep.




