
Diabetic retinopathy is a common eye complication that may affect the eyes of a diabetes patient. It is majorly caused by damage incurred to the blood vessels of a diabetic’s eyes.
However, this condition can be both treated and partly prevented if a person efficiently controls his or her blood sugar levels.
Initially, it may have zero symptoms or could appear as slight vision problems. Eventually, it can lead to complete or partial blindness. Diabetic retinopathy can occur in anyone who has either type 1 or type 2 diabetes. The longer you have had diabetes and less controlled your blood glucose is, the greater are your chances of developing this eye condition. Keep reading to know more about this disabling eye condition.
Table of Contents
- Symptoms
- Causes and Types of Diabetic Retinopathy
- Risk factors for Diabetic Retinopathy
- Prevention of Diabetic Retinopathy
- Diagnosis of Diabetic Retinopathy
- Treatment of Diabetic Retinopathy
- Health Complications Due to Diabetic Retinopathy
- Conclusion
Symptoms of Diabetic Retinopathy
You might not observe any symptoms in the initial stages of diabetic retinopathy. As it progresses, diabetic retinopathy may include the following signs and symptoms:
- Dark strings or spots floating in the vision (floaters)
- Blurred vision
- Fluctuations in your vision
- Impaired color vision
- Empty or dark areas in your vision
- Vision loss
This eye condition generally affects both the eyes. Let’s understand its causes and types.
Causes and Types of Diabetic Retinopathy
High sugar levels in your bloodstream can cause blockage of the blood vessels that nourish the eye’s retina, thereby cutting off the blood supply. To mitigate the damage, the eyes try to grow out new blood vessels. However, these tiny blood vessels don’t develop effectively and may leak out.
It can be classified into two types:
Early Diabetic Retinopathy:
This is a commonly seen type of diabetic retinopathy and is also known as non-proliferative diabetic retinopathy (NPDR). In this type no renewal of new blood vessels happens. The walls of blood vessels in the retina begin to weaken. Tiny bulges or microaneurysms protrude out from the vessel walls and at times leak blood and other fluids into the retina.
Advanced Diabetic Retinopathy:
This is more severe type and called proliferative diabetic retinopathy. In this, the damaged blood vessels lead to the growth of new blood vessels in eye’s retina. These blood vessels may leak fluids and blood into clear, jelly-like substance that fills the center of the eye. All of these might result in glaucoma.
Risk factors for Diabetic Retinopathy
Any person living with diabetes may develop diabetic retinopathy. Your risk of developing diabetic retinopathy may increase due to:
- Duration of your diabetes the longer you have had diabetes, the more is your risk of developing this eye condition
- Poor control of your blood sugar level
- High blood pressure
- Pregnancy
- High cholesterol
- Tobacco use
- Being Hispanic, African-American or Native American
Prevention of Diabetic Retinopathy
You might be not able to completely prevent diabetic retinopathy. However, managing you blood sugar and blood pressure, regular eye examination and early detection of vision problems may prevent severe or complete vision loss.
If you are a diabetic, you may prevent diabetic retinopathy by following the below recommendations:
Control Your Diabetes:
Eat healthy and indulge in physical activity to manage your diabetes. Try to work out for at-least 150 minutes every week. Always take your oral diabetes drugs and insulin as directed by your physician.
Closely Monitor Your Blood Sugar Levels:
You should keep checking and recording your blood sugar level few times each day. You need to take few more measurements in case you are under stress or are unwell. Get your hemoglobin A1C test done, periodically.
Keep Your Cholesterol Levels and Blood Pressure Under Control:
Losing excess weight, consuming healthy foods and exercising regularly will help you in managing your cholesterol levels and blood pressure. At times, medication is also required.
Quit Smoking:
Smoking isn’t good for your health and can make you vulnerable to various health complications including retinopathy.
Notice Your Vision Changes:
If you experience any drastic vision changes or you vision becomes increasingly blurry, you should see your eye doctor immediately.
Remember, diabetes would not necessarily result in vision loss. Managing your diabetes is the first step towards preventing various diabetes complications. Let’s learn how this eye condition is diagnosed.
Diagnosis of Diabetic Retinopathy
Diabetic retinopathy can be easily diagnosed by a comprehensive dilated eye exam. During this exam, specific eye drops are placed in your eyes to widen or dilate your pupils. This allows the doctor to view the inside your eyes easily. The drops might lead to blurry vision for several hours.
The eye doctor would look for the following changes:
- Any abnormal blood vessels formation
- Fatty deposits, blood or swelling in your retina
- Growth of any scar tissue
- Bleeding in jelly-like, clear substance that fills up the eye’s center (vitreous)
- Retinal detachment
- Changes in the optic nerve
Additionally, your doctor may also:
- Test your vision
- Measure the eye pressure to diagnose glaucoma
- Look for cataracts
Fluorescein Angiography:
The eye doctor might also take pictures of the insides of your eyes, when your eyes are dilated. He or she would then inject a special dye into one of your arm’s vein and take few more pictures when the dye circulates through the eyes’ blood vessels. These images would help in figuring any blood vessels that have closed, broken or are leaking fluid.
Optical Coherence Tomography:
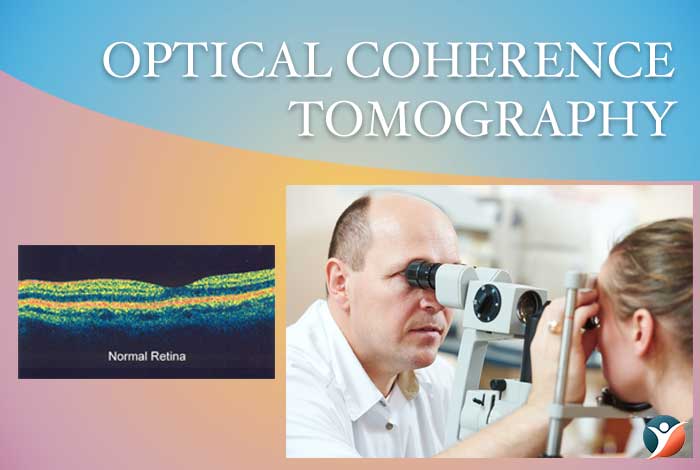
Your eye doctor might also ask for an optical coherence tomography (OCT) examination. This imaging test provides the cross-sectional images of your retina which can show the actual retinal thickness. This would also help in determining any leaked fluids in the eye. Later, OCT imaging may help in analyzing treatment’s effect.
With this, let’s get to the treatment available for diabetic retinopathy.
Treatment of Diabetic Retinopathy
Treatment largely depends on the type of diabetic retinopathy you have developed and severity of your condition. Treatment may include the following.
Early Diabetic Retinopathy:
If you have moderate or mild non-proliferative diabetic retinopathy, you might not require any treatment initially. However, your doctor will closely examine your eyes to figure out when you need treatment. You should work towards better diabetes management.
Advanced Diabetic Retinopathy

If you have developed proliferative diabetic retinopathy or what is commonly known as macular edema, you might require a prompt surgery. The following options may be considered:
Photocoagulation:
This is a minimally invasive laser treatment and also called focal laser treatment. Photocoagulation can halt or slow the fluid and blood leakage in the eye. During this procedure, fluid leaks from the abnormal blood vessels are halted with laser burns.
Pan retinal Photocoagulation:
This laser treatment is also commonly known as the scatter laser treatment. This can significantly shrink all the abnormal blood vessels. During this procedure, the areas of your retina that are away from macula are cured with scattered laser burns.
Vitrectomy:
This procedure involves making a tiny incision in the eye to remove all the accumulated blood from the vitreous part. This procedure is conducted in a surgery room or hospital under either local or general anesthesia.
Injecting Drugs into Your Eye:
Your eye doctor may recommend injecting certain drugs into the vitreous of your eye. These medications are known as vascular endothelial growth factor (VEGF) inhibitors and can inhibit growth of the newly formed blood vessels. Your doctor might also recommend anti-VEGF therapy to you alone or in combination of any above-mentioned surgery.
Even after a surgery and proper treatment of retinopathy, you may still require regular eye examinations.
Health Complications Due to Diabetic Retinopathy
Diabetic retinopathy leads to the growth of abnormal new blood vessels in the eye’s retina. This may lead to the below-mentioned vision problems:
Vitreous Hemorrhage:
The newly formed blood vessels might bleed into the substance that fills center of the eye. If bleeding is little, you might just see a few black spots (floaters). In severe cases, blood may completely fill the vitreous cavity and hamper your vision.
Retinal Detachment:
The abnormal blood vessels somehow stimulate growth of the scar tissue, which may pull out retina from the back of your eye. This may lead to floating spots in your vision, light flashes or extreme vision loss.
Glaucoma:
New blood vessels might begin to interfere with normal fluid flow out of your eye, thereby resulting in pressure build up (glaucoma). This extra pressure may damage the optic nerve which carries images to the brain.
Blindness:
Diabetic retinopathy or glaucoma or both may result in complete vision loss.
Conclusion
Fortunately, lifestyle changes like consuming a healthy diet, exercising regularly, losing excess weight, and quitting smoking may help in managing your diabetes and mitigate the chances of developing retinopathy. You might also be recommended medications to manage your diabetes and regular eye examinations. Simply put, diabetes retinopathy can be partly prevented and treated with proper medical intervention. With proper diabetes management, you can prevent development of any eye condition associated with diabetes.
Did you enjoy reading our article? Did you follow any of our recommendations? Leave your feedback and recommendations in the comment section below. We will keep you posted with latest information, right here. Keep checking out this space for more on diabetic retinopathy.




