Diabetes has emerged as the largest epidemic in the recent times and people often wonder about diabetes etiology and pathogenesis. In the recent times, a concept has emerged that diabetes mellitus is not a single disease but rather a bunch of symptoms which are characterized by inappropriately elevated fasting and after meal blood glucose levels. This causes development of long-term changes in the body which causes a deterioration in the overall health of the patient. On taking a closer look at the genetics, epidemiology, causes and how the disease affects the body, these inferences have been drawn. Read on to discover the complete guide on the etiology and pathogenesis of the disease that is plaguing the entire world.[1]
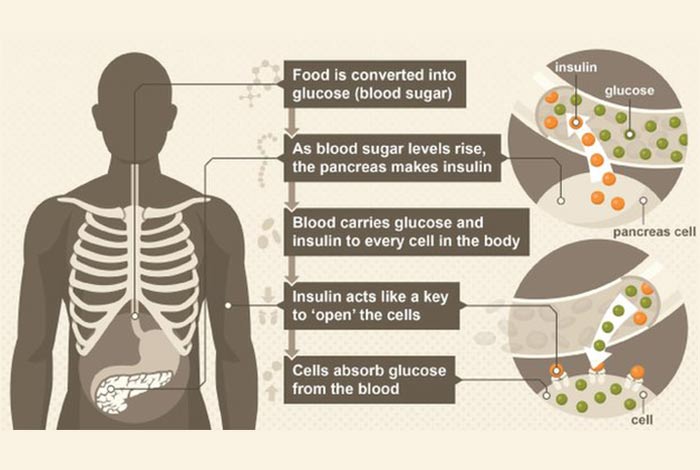
Diabetic Mellitus refers to a group of disorders in which abnormal carbohydrate metabolism leads to elevated blood glucose levels. Each individual has his own reason why there is a relative or absolute impairment and resistance to insulin in the body. When the body is unable to synthesize insulin, it leads to development of insulin-dependent diabetes. When the body develops resistance against insulin, it leads to development of insulin-independent diabetes.
The Expert Committee on the Diagnosis and Classification have revised the basis on which diabetes is diagnosed. When the blood glucose levels from two consecutive tests show fasting blood glucose levels more than 126 mg/dL (> 7mmol/L), it is diagnosed as diabetes without any apparent symptoms.
As per the guidelines, the normal fasting blood glucose level has been dropped from 110 mg/dL to 100 mg/dL, which implies that anyone with a fasting blood glucose above 100 mg/dL will be diagnosed as having an impaired fasting glucose (IFG). Those people with IFG levels between 100-125 mg/dL are at a high risk of developing diabetes and should get their blood glucose regularly monitored.
More recently, American Diabetes Association has recommended the use of HbA1C test [2] for determining whether a person has diabetes or not.
| Glucose Level | ADA Evaluation |
| Normal |
|
| Impaired Fasting Glucose (IFG) |
|
| Impaired Glucose Tolerance (IGT) |
|
| Diabetes Mellitus |
|
| HbA1C |
|
Table of Contents
- Etiological Classification of Diabetes Mellitus
- Genetic Defects in Insulin Action
- Endocrinopathies
- Drug or Chemical Induced Diabetes
- Viral Infection
- Uncommon Forms of Immune-Mediated Diabetes
- Conclusion
Etiological Classification of Diabetes Mellitus
1. Type I Diabetes Mellitus
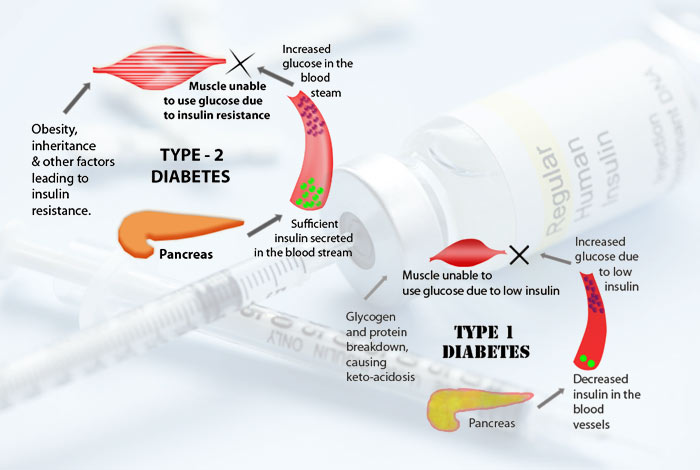
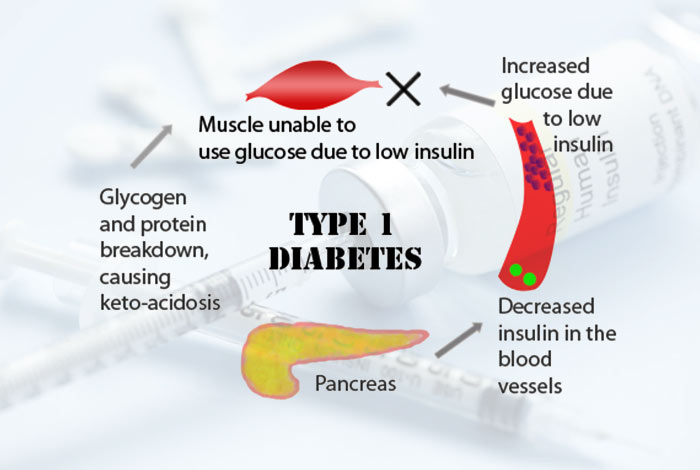
Type I diabetes mellitus is caused by a number of reasons that effect the beta cells of pancreas and results in ultimate deficiency of insulin in the body. These reasons can be destruction of beta cells of pancreas by the immune system of the body or some underlying defects in the insulin secretion which is often inherited from the parents.
2. Type II Diabetes Mellitus
It is one of the most common forms of diabetes and is characterized by development of insulin resistance in the body. In this disease, insulin is unable to show its action on target tissues like liver, muscle and fat. With time, there is progressive failure of beta cells which damages their insulin secretion capacity. Most patients of type II diabetes in Europe and the U.S.A. have obesity, however, in India and China, a lean BMI is observed with increased visceral fat. This indicates that obesity results from insulin resistance in the body. Obesity is not the cause of diabetes.
3. Monogenic Diabetes
Monogenic diabetes occurs when a single mutation occurs in the gene which results in dysregulation of glucose level in the body.[3]
This disorder is inherited by the child from either or both of his parents. In other cases, the mutation can occur spontaneously which implies that it is not inherited by the child from either of his parents. Most of the mutations that result in monogenic diabetes decrease the body’s ability to synthesize insulin. It is of following types:
a. Permanent Neonatal Diabetes
Neonatal jaundice is a rare genetic disorder in which an infant develops diabetes in the first 6 months of life and the severity of the disease depends on the underlying mutation that is present in the body.
b. Mitochondrial diabetes
When a single gene mutation occurs in mitochondrial genetic material, it results in impairment in insulin secretion. This causes hearing problems along with diabetes. This type of diabetes is passed on from mothers to her children. In this the person has difficulty in converting pro-insulin into insulin or there is production of faulty insulin.
c. Maturity Onset Diabetes of the Young
Maturity onset diabetes of the young is a rare form of diabetes that is known to run in families. It occurs when there is a mutation in a single gene which results in the development of diabetes. This mutation results in disruption of insulin production in the body which causes blood glucose level to go haywire. There are a number of types of MODY which depends on the kind of mutation that occur in the person.[4]
d. Chronic Illness
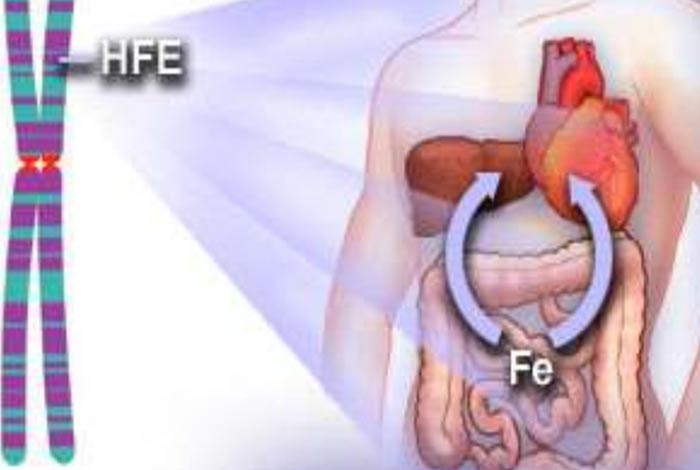
(I) Hemochromatosis:
Hemochromatosis refers to a disease in which excessive accumulation of iron occurs in different body organs like liver, pancreas and heart. Without treatment, the organ gets damaged and lead to development of several diseases like diabetes, heart diseases and cirrhosis.
This is a more common cause of diabetes that occurs with progressing age.
(ii) Cystic Fibrosis:
Cystic fibrosis is a progressive genetic disease that results in persistent lung infection and decreases the ability to properly breathe with time. In these people, there is a defective gene which causes a buildup of mucus in pancreas, lungs and other organs. Mucus in the pancreas prevents the release of enzymes and hormones from it. Insulin is one such hormone that gets released from pancreas whose action is to decrease blood glucose level in the body. In people with cystic fibrosis, there is decreased secretion of insulin which leads to development of diabetes.
(iii) Gitelman’s Syndrome:
This is a genetic disease of kidney in which there is decreased levels of potassium and magnesium, elevated blood pH and reduced excretion of calcium in the urine. In these patients magnesium deficiency develops which gives rise to diabetes. However, when magnesium levels were restored in the body, diabetes symptoms were seen to get improved.
4. Genetic Defects in Insulin Action

A number of rare genetic abnormalities can occur in the insulin receptor that can hinder proper attachment of insulin to it. When insulin does not get attached to the receptors, the cells cannot take up insulin from the blood which results in increase in blood glucose level. Also, if a person has a genetic disease known as Bloom’s Syndrome, the body will have severe insulin resistance. Other genetically arising conditions that also cause diabetes are progeria and lipodystrophy.
5. Endocrinopathies
It refers to a disease of endocrine gland which results in disbalance of hormones in the body. In some people with diseases in the endocrine gland results in development of insulin resistance in the body which is secondary in nature. Such diabetes is moderate in nature and presents itself with symptoms of glycosuria, hyperglycemia and others.
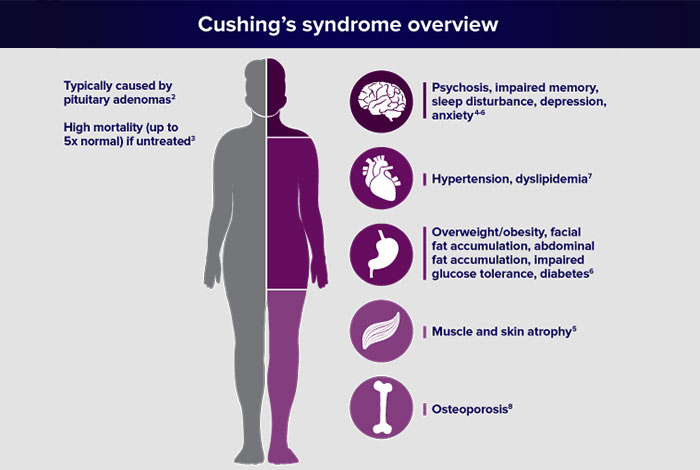
a. Cushing Syndrome
Prolonged and excessive levels of cortisol hormone occur in Cushing Syndrome due to development of tumor. Cortisol is natural stress hormone and is released in emergency situations. It causes an increase in blood sugar. When tumor develops, it causes an excessive increase in blood sugar level which takes the form of diabetes. It is often seen in people who have pre-existing insulin resistance.
b. Acromegaly
Acromegaly results when there is excessive production of growth hormone after the growth plates have closed. Growth plates is a hyaline cartilage plate that is present between two long bones and is the region where growth occurs. In 10-15% people with over diabetes, acromegaly is observed. In these people marked insulin resistance and hyperinsulinemia is also seen which results in impaired glucose tolerance.
c. Pheochromocytomas
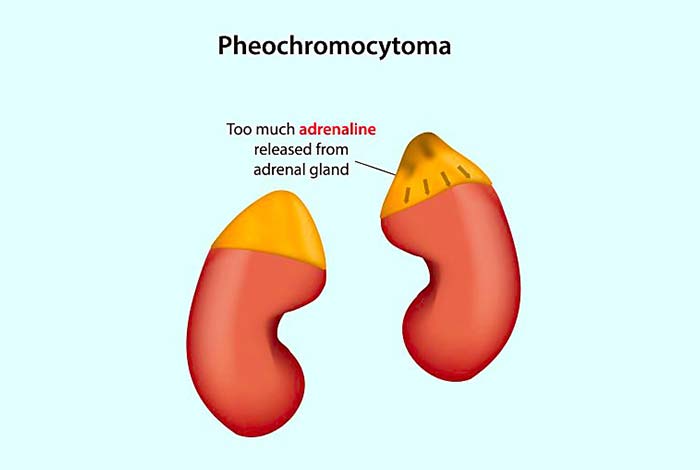
This is a disease in which a rare tumor develops in the adrenal gland which secretes adrenaline and results in elevation of blood pressure. It affects one or both of the adrenal glands and if left untreated, can result in severe or life-threatening damage to other organs of the body as well, like pancreas.
Pheochromocytomas inhibit the secretion of insulin secretion and an increase in the glucose production by the liver. These changes cause impaired glucose tolerance in the body whose severity depends on the amount of hormone produced by the tumors. When pheochromocytoma is observed in children, it is often a component of Von Hippel -Lindau Syndrome.
d. Glucagon- secreting tumors (Glucagonoma)

Glucagonoma is a rare tumor that originates in the pancreas in which the islets of Langerhans get affected. These cells are responsible for the endocrine function of the pancreas and contains a number of cells, namely alpha, beta and delta that secrete different hormones, insulin being one of it.
People with glucagonoma display a number of clinical features like weight loss, anemia and thromboembolic problems. Nearly 80% patients either have diabetes or glucose intolerance.
e. Somatostatin- secreting tumors (Somatostatinomas)
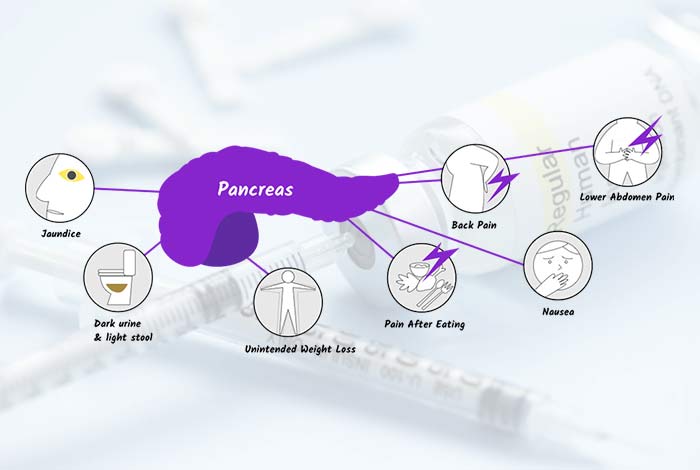
In this, a tumor develops in the delta cells of the endocrine portion of the pancreas that synthesizes somatostatin, which is the growth-hormone inhibiting hormone. Somatostatinomas are associated with the triad of gallstones, diabetes mellitus and diarrhea with steatorrhea.
f. Hyperthyroidism
Hyperthyroidism is a disease in which the thyroid gland produces excess of thyroid hormone, thyroxine. Hyperthyroidism is known to interfere with the metabolism of glucose in the body. There is increased sensitivity of pancreatic beta cells to glucose which causes an upsurge in the secretion of insulin and also hinders its action.
6. Drug or Chemical Induced Diabetes
Some of the drugs that are known to impair glucose tolerance. These drugs might act by:
- Reducing the insulin secretion
- Escalating glucose production in liver
- Inducing resistance to the action of insulin
Following classes of drugs are responsible for causing the above-mentioned effects:
a. Antihypertensive drugs that are responsible for lowering blood pressure
- Beta blockers
b. Protease inhibitors that are used in the treatment of HIV
c. Immunosuppressants that are given after organ transplant
- Tacrolimus
- Cyclosporin
d. Serotonin reuptake Inhibitor (SSRI)
e. Thiazide diuretic or Beta blocker in a patient of Metabolic Syndrome
7. Viral Infection

Certain viruses are also known to cause diabetes either through direct destruction of cells of immune system or by inducing an auto immune response in which the immune system starts attacking the body’s own cells. These viruses are:
- Coxsackie B4
- Chronic Hepatitis C virus
8. Uncommon Forms of Immune-Mediated Diabetes

a. Stiff- Man Syndrome: It is an autoimmune discover in which the immune system of the body starts attacking the central nervous system and damages it. The disease most commonly presents itself in the early adulthood. Grave’s disease is also seen to occur simultaneously in these patients, in which there is excessive production of thyroid hormones.
b. Anti-Insulin Receptor Antibodies
These antibodies can bind to insulin receptors and can either increase the action of insulin due to which glucose level falls in the blood or can inhibit the action of insulin altogether thereby resulting in diabetes. This type of insulin resistance is commonly seen in females who show other symptoms of autoimmune diseases as well like systemic lupus erythematosis (SLE).
c. IPEX Syndrome
It is caused by a rare mutation due to which permanent neo-natal diabetes occurs.
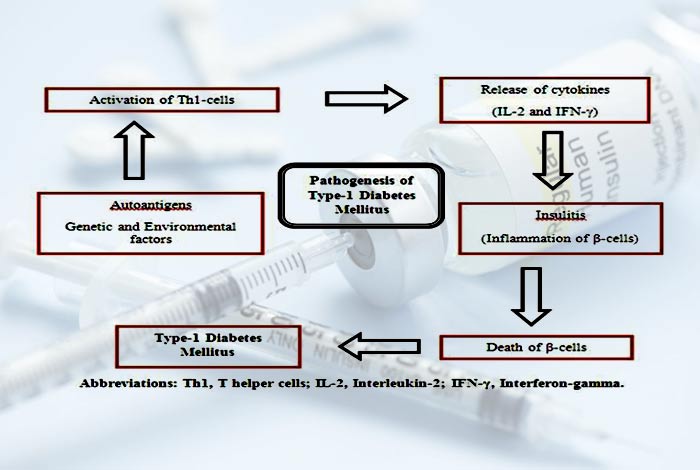
Pathogenesis of Type I Diabetes
In type I diabetes, the destruction of beta cells occur that is chronic in nature. It often begins during infancy and continues to grow as the time passes by. At the time of diagnosis, nearly 80% of the beta cells have been destroyed and the islets are infiltrated by inflammatory cells that result in the development of insulitis.
Once the islet cell autoimmunity begins, there is a variable progression to islet cell destruction, in some, the destruction can occur rapidly while in others it can be slow.
The exact mechanism by which beta cell destruction occurs is unclear. The development of beta cell specific antibody is considered the first step that leads to development of the disease. Then later on, several other chemicals also start developing that further damage the beta cells. Prolonged damage to beta cells results in development of diabetes.
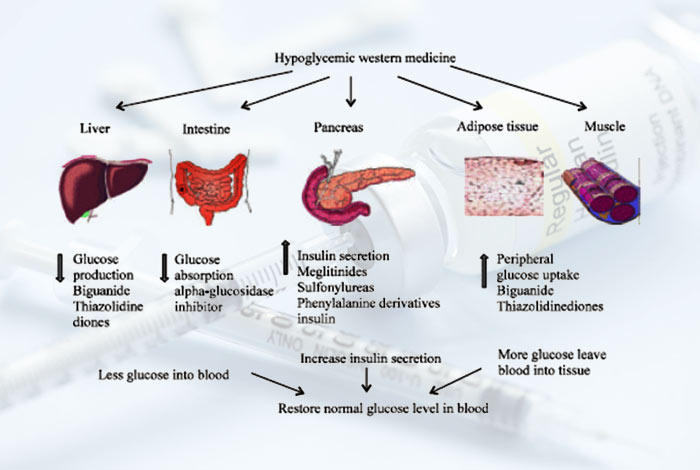
Pathogenesis of Type II Diabetes
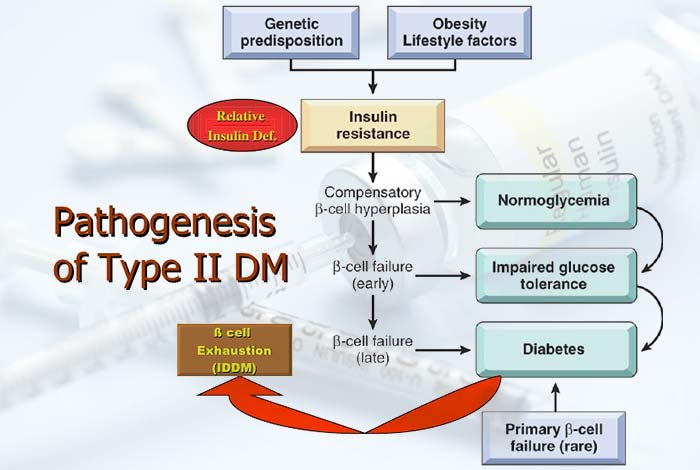
In type II diabetes, the peripheral tissues like fat, muscles and liver develop insulin resistance due to which glucose cannot be absorbed from the blood. Along with this, there is progressive failure of beta cells, reduction in the secretory properties of pancreas in response to glucose, escalation in production of glucose by liver and no pancreatic autoimmunity. All these factors lead to the development of type II diabetes.
| Factor | Effect |
| Intrauterine environment | Strong association is observed between poor intrauterine growth and development of metabolic syndrome. Poor nutrition in the early days of life impaired the development of pancreas and caused permanent changes in the glucose-insulin metabolism |
| Gestational diabetic | If the expectant mother had diabetes at the time of pregnancy, there is an increased chance for the offspring to develop diabetes later in life. |
| Ethnicity | Some races and ethnic groups have an increased risk of developing diabetes |
| Gender and Puberty | At the time of puberty, there is development of insulin resistance and a 30% decrease in insulin sensitivity is observed. Also, there is compensatory increase in insulin production by the pancreas.
Girls are 1.5 to 3 times more likely to develop type II diabetes in childhood than boys when they are at the peak of adolescent growth. |
A person with type II diabetes develops insulin resistance while there is a fall in the disposition index, which is the amount of insulin produced for the amount of insulin resistance developed in the body. Gradually the glucose levels of the body start to increase after consuming a meal and later on, even the fasting blood glucose level goes haywire. At this stage, precautionary mechanisms like diet and exercise are suggested. Later, medicines that increase the secretion of insulin are prescribed in order to keep blood glucose levels in check.
Insulin Resistance Syndrome

This syndrome is centered around the genetic vulnerability of a person to develop resistance against insulin and the subsequent development of hyperinsulinism. This medical state is also known as syndrome X and the metabolic syndrome. It is thought to run in families and therefore is considered to have a dominant nature.
Affected patients often have polyphagia and therefore develop obesity. They often have voracious appetite that shows resistance to any dietary advice. They shoe deficiency of a hormone, called leptin which is responsible for the development of obesity. There is also development of non-alcoholic fatty liver syndrome in these patients.
Gestational Diabetes
Insulin resistance and impaired function of beta cells contribute to gestational diabetes. There is impaired sensitivity to insulin during pregnancy. This type of diabetes general develops as the expectant mother enters second trimester of pregnancy. Placental hormones, progesterone, prolactin and several other hormones are responsible for development of gestational diabetes. They change the insulin receptor which results in the development of profound insulin resistance in the body. Technically, the pancreas should compensate for the increase in demands of insulin by the body but this is not observed as there is reduction in the function of beta cells. This feature is contributed by the development of autoimmunity.
Pathogenesis of MODY
Maturity -onset diabetes of the young is caused by a mutation in a single gene that leads to dysfunction of beta cells of the pancreas. However, since it is not possible to get beat cells from a patient easily or ethically for carrying out experiments, the exact pathogenesis of MODY in humans is not understood completely. All that can be made out from the limited data that is available is that there is generation of disease specific induced pluripotent stem cells (iPS) which cause the gene to dysfunction.
Conclusion
Diabetes is a disease that can only be managed and has no cure till date. However, with new discoveries being made each day, there is increasing hope for the patients.