
Overview and Facts
Chronic obstructive pulmonary disease or COPD is a group of progressive respiratory diseases that cause difficulties in breathing – a process by which the air gets in and moves out of the lungs.
To better understand COPD, it is important to understand the process of breathing or respiration. The air inhaled by a person travels through the trachea or windpipe into the lungs via two large bronchial tubes. These tubes divide inside the lungs into several smaller branches, known as bronchioles. These bronchioles terminate at clusters of air sacs or alveoli. These air sacs have very thin walls full of blood capillaries. The oxygen from inhaled air is passed to the bloodstream through these capillaries. Simultaneously, carbon dioxide which is a waste product of body’s metabolism is exhaled.
As already stated, COPD is a cluster of several respiratory conditions. The most common conditions include chronic bronchitis and emphysema. Many people suffering from COPD have both these conditions. Chronic bronchitis is inflammation in the lining of bronchial tubes. Common symptoms of chronic bronchitis are excessive mucus production and cough.
Similarly, emphysema is a condition, wherein alveoli are destroyed due to overexposure to cigarette smoke, particulate matter and other lung irritants. The general symptoms of COPD are cough, wheezing, breathing difficulty and excessive mucus production. These symptoms are initially milder, but as COPD progresses, it makes it extremely hard to breathe. There are four stages of COPD:
- Stage 1: Very mild – with chronic cough and mucus production,
- Stage 2: Moderate – with chronic cough, excessive mucus production and shortness of breath
- Stage 3: Severe – with frequent flare up and exacerbations
- Stage 4: Very severe – with life-threatening flare-ups.
Sadly, there is no specific cure for COPD, but treatment can help in reducing the symptoms, lowering the chance of complications and improving the quality of life. If left untreated, it might also lead to several heart problems, respiratory infections, pulmonary hypertension, depression and even lung cancer.
The World Health Organization (W.H.O) estimates that around 65 million people around the globe suffer from moderate to severe COPD.[1] According to the Centers for Disease Control and Prevention (CDC), there are around 15.7 million adults, who have been diagnosed with COPD and more than 50% of the people with COPD are not aware of their condition in the U.S.[2] Most people suffering from COPD are aged 40 years or older.[3] Smoking is the leading cause of COPD and around 20- 30% of all chronic smokers develop it at some point of life.
According to the National Institute of Health (NIH), around 120,000 die of COPD each year in the U.S.,[4] making it the third leading cause of death in the country.[5] More women die of COPD than the men. It has been estimated that COPD cases will increase by more than 150% between the year 2010 and 2030.[6]
Types and Symptoms of COPD
Types of COPD:
Mainly, there are two forms of COPD – chronic bronchitis and emphysema.
- Chronic Bronchitis: Bronchitis is inflammation of the bronchial tubes that bring air to and from the lungs. Due to the inflammation, the internal lining or mucus membrane grows thicker or swells. This increased thickness and mucus together obstruct the air passage and causes a phlegmy cough. General symptoms of chronic bronchitis are wheezing, shortness of breath, fatigue, chest tightness and frequent respiratory infections. These symptoms might worsen during increased levels of pollution and smog.
- Emphysema: Emphysema occurs when the alveoli or air sacs of the lungs get damaged and enlarged. These damaged air sacs lose their normal elasticity and lead to difficulty in breathing. The narrowed bronchioles and inelastic alveoli do not allow the air to fully expel out. This might result in ruptured alveoli, decreased surface area for gaseous exchange and reduced number of alveoli. Its common symptoms are wheezing, shortness of breath, frequent respiratory infections, fatigue, reduced appetite and weight loss.

Symptoms of COPD:
The early symptoms of COPD can often be mistaken for common cold. These symptoms are:
- shortness of breath; mostly after physical exercise
- mild, but recurrent coughing
- clearing throat often, especially the first thing after waking up
As the condition progresses, the symptoms gradually worsen due to lung damage. The symptoms might be:
- shortness of breath after climbing a flight of stairs
- noisy breathing or wheezing
- tightness in chest
- chronic cough with or without mucus
- need to eliminate mucus from lungs everyday
- frequent flue, cold and other respiratory infections
- weakness or loss of energy
In the severe or later stages of COPD, the symptoms might be:
- fatigue
- appetite loss
- weight loss
- swelling of the legs, feet or ankles
- fever along with common cold or flu symptoms
- restlessness, forgetfulness, confusion, slurring of speech, or irritability
- extreme fatigue or unexplained weakness that lasts for more than a day
Immediate medical attention should be provided if:
- a person has gray or bluish fingernails or lips as these indicate low oxygen level in the blood
- a person cannot talk due to breathlessness or a racing heart
- a person feels confused or faint
People suffering from COPD might also experience exacerbations, wherein they might have worsened symptoms that might last several days.

Risk Factors for COPD
There are several risk factors for COPD. These include:
- Smoking: Long-term cigarette smoking is a significant risk factor for COPD. The more cigarette packs and more years a person smoke, the greater is the risk to develop COPD. Marijuana smokers, pipe smokers and cigar smokers are also at an increased risk along with those, who are regularly exposed to second-hand smoke.
- People with Asthma Who Smoke: People who are already suffering from asthma – a chronic and inflammatory airway condition – and smoke, increases their risk of developing COPD.
- Occupational Exposure to Chemicals and Dust: Long-term exposure to chemical fumes, vapors and particulate matter at workplace can leave lungs inflamed and swelled. This increases the risk of developing COPD and other respiratory conditions.
- Exposure to Fumes of a Burning Fuel: People, who are exposed to burning fuel during heating or cooking in poorly ventilated homes, mostly women, are at an increased risk of developing COPD.
- Age: COPD generally develops as one ages. For this reason, most people observe its symptoms for the first time as they enter their 40s.
- Ethnicity: According to the statistics on COPD, non-Hispanic Whites are at a greater risk of developing COPD.
- Genetics: The rare genetic disorder alpha-1-antitrypsin deficiency (AATD) has been found to be a causative factor in several cases of COPD. Several other genetic factors might make smokers more prone to develop COPD.

Do I have COPD?
If you experience:
- Shortness of breath that occurs more often or has worsened
- Excess mucus buildup
- More and frequent wheezing or coughing
These symptoms might indicate COPD or several other conditions, such as obstruction of the lung airways, asthma, bronchiectasis, chronic bronchitis, emphysema, bronchiolitis, interstitial lung diseases, coronary artery disease, pulmonary edema, or pulmonary embolism.
Therefore, one must visit a doctor immediately to diagnose the exact condition, responsible for these symptoms. Only a doctor can diagnose COPD through several tests and initiate the treatment accordingly.

Causes and Prevention of COPD
Causes of COPD:
Major causes of COPD are discussed below:
- Smoking: Smoking is the leading cause of COPD. Around 9 in every 10 cases of COPD are smokers or have a history of smoking. The toxic and harmful chemicals in smoke can inflame and damage the lining of the lung airways. Cessation of smoking can help in preventing COPD to worsen. Also, being exposed to passive smoke can lead to the development of COPD.
- Dust and Fume Exposure at Workplace: Exposure to certain types of chemicals, dust and fumes at the site of work might lead to the development of COPD. Substances that have been linked with COPD are silica dust, welding fumes, grain or flour dust, isocyanates, coal dust, cadmium dust and fumes.
- Genetics: A person, who smokes and has a close family member suffering with COPD is more prone to develop COPD. Around 1 in 100 people have a rare genetic condition, called alpha-1 antitrypsin deficiency, which makes such people more vulnerable to lung damage. Alpha-1 antitrypsin (a protease enzyme inhibitor) helps in protecting lungs, and its deficiency causes lung damage and might even lead to COPD. People, who have its deficiency and also smoke, generally develop COPD around the age of 35 years.
Prevention of COPD:
Several preventive measures can be taken to manage the symptoms of COPD. These are discussed below:
- Cessation of Smoking: COPD is strongly linked with smoking. It can be prevented by quitting smoking. If a person is a heavy smoker and has failed to quit, he/she must keep trying to quit smoking. If necessary, a person willing to quit smoking can also join a tobacco cessation program to quit. It is also advised to avoid second-hand smoke or passive smoking to prevent COPD.
- Avoid Fumes and Dust Exposure at Workplace: A person, who is constantly being exposed to dust and chemical fumes at workplace must take measures to prevent the exposure. Use of respiratory protective equipment can help prevent exposure to harmful fumes and particulate matter.

Diagnosis and Tests for COPD
At times, COPD is misdiagnosed and smokers, who are actually suffering from mild deconditioning of lungs are told that they have COPD. Also, in several cases, COPD is not diagnosed until it reaches its advanced stages and becomes more resistant to treatment.
To properly diagnose COPD, the doctor asks details about the symptoms, their severity and frequency. Also, the doctor may ask about a person’s medical as well as family history and inquire about the patient’s history of exposure to lung irritants, such as cigarette smoke. The tests conducted to diagnose COPD include:
- Pulmonary (Lung) Function Tests: These tests measure the amount of air a person can inhale or exhale and whether the lungs are providing an adequate amount of oxygen to the blood. Spirometry is a common pulmonary function test. During spirometry, a person is asked to blow air into a small device, known as spirometer. The machine measures how fast a person can blow out air and how much air the lungs can hold.
Spirometer is effective in detecting COPD even before the symptoms surface. This is often used to check the progression of the disease and the effect of treatment. Besides, lung function tests also help in measuring pulse oximetry, diffusing capacity and lung volume.
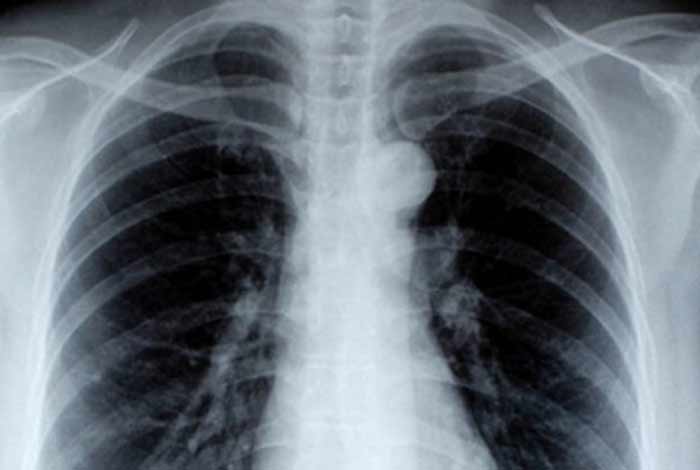
- Chest X-Ray: A chest X-ray can show emphysema. An X-ray can also rule out any other lung problems or even a heart failure.
- CT Scan: A CT scan can help detect emphysema and whether a person can be benefited with surgery. These scans also help in the screening of lung cancer.
- Arterial Blood Gas Analysis: This analysis involves a blood test to measure how well the lungs are bringing oxygen to the blood and removing carbon dioxide from the same.
- Laboratory Tests: These tests do not help detect COPD but may help finding the underlying cause of the symptoms. For example, laboratory tests to identify alpha-1 antitrypsin deficiency (AATD) in a person, which might cause COPD in future. These tests might be conducted if a person develops COPD before the age of 40 or he/she has a family history of COPD.
Treatment and Care for COPD
Treatment for COPD:
The treatment of COPD involves medications, lung therapies and in very extreme cases, surgery. A combination of medications and therapies might be helpful in moderate to severe cases of COPD.
Even in advanced stages of COPD, there is an availability of effective therapy, which can prevent worsening of symptoms, reduce the exacerbations and provide a better quality of life. The treatment options for COPD are as follows:
1. Medications: The doctor might prescribe several medications to control the symptoms of COPD. A few of these medications are to be used regularly while some are used as required. These medications are:
- Bronchodilators: These medications relax the muscles around the lung airways and are usually available in the form of inhalers. Bronchodilators help in relieving the shortness of breath and coughing; thereby, easing the breathing.
Depending on the severity of COPD, a person might require a short-acting bronchodilator before any physical activity or a long-acting bronchodilator every day, or both if required.
The long-acting bronchodilators are salmeterol, tiotropium, arformoterol, formoterol, aclidinium and indacaterol, whereas short-acting bronchodilators include levalbuterol, ipratropium and albuterol.
- Inhaled Steroids: Inhaling corticosteroid medications can help reduce inflammation in the lung airways and prevents future exacerbations. Side effects of inhaled steroids are hoarseness, oral infections and bruising. These are mostly used by people, who experience frequent exacerbations of COPD. Budesonide and fluticasone are examples of inhaled corticosteroids.
- Combination Inhalers: Several medications have a combination of inhaled steroids and bronchodilators. Fluticasone and salmeterol, and budesonide and formoterol are the examples of combination inhalers.
- Oral Steroids: If a person is suffering from moderate or severe acute exacerbations, they are prescribed with a short course of oral corticosteroids. Long-term use of oral steroids might cause infections, weight gain, cataracts, diabetes and osteoporosis.
- Phosphodiesterase-4 Inhibitors: People with chronic bronchitis and severe COPD are sometimes prescribed these phosphodiesterase-4 inhibitors. Roflumilast is one such phosphodiesterase-4 inhibitor. It reduces inflammation in the lung airways and relaxes the airways. Common side effects of this medication are weight loss and diarrhea.
- Theophylline: This medication might help in preventing exacerbations and improving breathing. Generally, lower doses are recommended because it might cause headache, tremor, nausea and fast heartbeat.
- Antibiotics: According to a recent study, azithromycin helps in preventing exacerbations. Antibiotics are used to treat acute exacerbations.
2. Lung Therapies: Doctors often use these additional therapies for patients with moderate to severe COPD. These may include:
- Oxygen Therapy: Supplemental oxygen is required when there isn’t enough oxygen in a person’s blood. There are several devices that provide the extra oxygen to a person suffering from COPD.
It includes small, lightweight portable devices that provide extra oxygen. Some people only require extra oxygen while performing any physical activity or sleeping. There are a few COPD patients, who require extra oxygen all the time. Oxygen therapy might extend life and can remarkably improve the patient’s quality of life. A doctor can help choose the best available option for a COPD patient.
- Pulmonary Rehabilitation Program: These rehabilitation programs comprise exercise training, education, counseling and nutrition-related advice. A variety of specialists create a custom program to meet all needs of a COPD patient. These pulmonary rehabilitation programs improve quality of life and help the patient to actively participate in daily activities.
3. Surgery: For people with severe emphysema, who hasn’t been benefited by medications, a doctor may suggest a surgery. The surgery options for these people are:
- Lung Volume Reduction Surgery: In this procedure, a surgeon removes damaged lung tissues from the upper part of lungs. This extra space helps daiphragm to work more efficiently and the healthier lung tissues expand to accommodate the additional space. This surgery can extend lifespan and improve quality of life.
- Lung Transplant: Certain people with COPD, who meet the established criteria for lung transplant undergo this surgery. It helps them in leading an active life with reduced or no breathing problems. However, they might have to take immune-suppressing medications for the rest of their life to prevent organ rejection.
- Bullectomy: If walls of the alveoli are destroyed, they might lead to the formation of large air spaces, known as “bullae” in the lungs. These bullae can become larger and might start causing difficulties in breathing. In a bullectomy surgery, the doctor removes bullae from the lungs to improve the airflow.

Care of People with COPD:
Following measures can be taken by a family member or caregiver to help the COPD patient manage his/her condition:
- Remind the patient to take medications on time and as prescribed by the doctor.
- Do not give cough suppressants to the COPD patient as coughing helps in eliminating excess mucus. Use of cough suppressants is generally not advised.
- Try to keep patient away from cold air as it can trigger shortness of breath and bronchospasm. Keep the windows and doors closed during cold weather.
- Encourage the patient to consume a well-balanced diet.
- Use an air humidifier in homes to help the patient breath properly.
- Remove the clutter and dust from your homes, so as to prevent the patient from inhaling such cough triggers.
- Learn as much as possible about COPD to understand the condition of the patient and to take better care of him.

OCT Medications and Self-Management methods available for COPD
Acetaminophen is a potent ingredient of numerous medications like cough suppressants and pain relievers. NSAIDs including naproxen, aspirin, and ibuprofen are common OTC medications used to relieve pains and reduce fever associated with COPD. They are also taken for allergies, colds and sinus pressure. Several other over-the-counter supplements like coenzyme Q-10, amino acids and antioxidant vitamins are known to be beneficial in improving the symptoms of COPD.

Self-Management Methods for COPD
A patient can effectively manage his/her symptoms by following the below-given tips:
- Lungs get weakened due to COPD. Avoid anything that might overtax the lungs or cause exacerbations.
- Quit smoking completely and also try to avoid second-hand smoke. If a person frequently fails to quit smoking, he/she must join a smoking cessation program.
- Exercising a little each day helps keeping the body and mind healthy. A doctor can advise on how much exercise is good for a person with COPD.
- Avoid pollutants, pollens, particulate matter and strong smells. Use respiratory masks to avoid exposure to workplace chemicals and fumes. Avoid being around construction sites.
- Consume a well-balanced diet that has high nutritional value. Avoid packaged and highly processed foods that are overloaded with calories and sugars.
- Limit the intake of salt as it can retain water and might strain breathing.
- Maintain a healthy weight according to your height.
- Include nutritious foods, such as dairy products, grains, fruits and vegetables in your daily diet.
- Consume around 8-10 glasses of water per day and only noncaffeinated drinks.
- It is important to manage other chronic diseases like diabetes and heart diseases if a person has these along with COPD.
- Keep homes dust and clutter free. Avoid letting the pets on bed. Organizing things would help in saving energy.
- Always carry emergency contact numbers along with the medications and their doses. Feed emergency contact numbers in your mobile phone.
- Join a support group which provides much needed motivation and inspiration to cope up with COPD.
- Maintain a journal and note down the triggers that lead to exacerbations. Reduce stress and anxiety through meditation and yoga.
- Avoid crowded spaces as being at such places can increase the risk of respiratory infections.
- Cover the nose and mouth with a cloth while getting out in cold, dust or fog. This helps prevent worsening of COPD symptoms.
- Implement several breathing techniques that help in breathing effectively.
- Sleep for at least seven hours a day. Keep regular with your wake time and bedtime.
- Avoid infections by regularly washing hands and getting vaccinated.
- Practice deep and huff coughing methods to expel excess mucus.

Natural Ways to Cure COPD
There are several natural ways to manage or prevent the symptoms of COPD. These include:
- Acupuncture: This is an ancient Chinese technique of inserting fine needles into the skin at special points, known as meridians. These are the points, where blockage of energy occurs. Acupuncture is known to be beneficial in reducing the symptoms associated with COPD. However, a person is advised to visit a licensed practitioner.
- Eucalyptus Oil: Eucalyptus oil is very beneficial in improving lung function and overall health of a person with COPD. Cineole is the main constituent of eucalyptus oil. It helps in reducing inflammation in the airways and shortness of breath. A person with COPD can use eucalyptus oil in an air humidifier or a diffuser and breath in the air.
- Ginseng: Ginseng is a natural herb which decreases the lung bacteria and improves lung function. In Chinese medicines, ginseng has been long used for treating respiratory conditions. Consuming ginseng helps in reducing the symptoms associated with COPD.
- N-Acetylcysteine (NAC): NAC supplements help in reducing the frequency and severity of COPD exacerbations and help in improving the overall lung function. NAC increases the level of glutathione, which fights against oxidative stress and thins the mucus in the lung airways.
- Vitamin D: Consuming milk and staying outside in the sun for a while helps in getting daily dose of vitamin D. It has been linked with better lung functioning. A person suffering from COPD can consume soy or almond milk rather than consuming regular milk as it can lead to excess mucus buildup.
- Antioxidant Vitamins: People with COPD, who consume foods that are rich in vitamin A, C and E have shown great improvements in their lung functioning. Increase intake of foods like carrots, cantaloupe, apricots, strawberries, broccoli, papaya, citrus fruits, kale, bell peppers, spinach, tomatoes, asparagus and other green leafy vegetables.
- Bromelain: Bromelain is a chemical produced by the enzymes present in pineapple stems. It reduces the inflammation in the lung airways and relieves symptoms of COPD. A person suffering from COPD can consume pineapple smoothie or juice to get adequate amount of vitamin C and bromelain.
- Coenzyme Q10: It is present in trace quantities in a variety of foods like mackerel, peanuts and sardines. Coenzyme Q10 helps in airway dilation due to its anti-inflammatory properties. It reduces the symptoms associated with COPD. A person with COPD can also consume supplements of coenzyme Q10.
- Breathing Techniques: A person with COPD is advised to practice various breathing techniques. Most commonly practiced breathing techniques are diaphragm and pursed lip breathing. A therapist or doctor can teach these techniques to a COPD patient.
- Relaxation Techniques and Meditation: Relaxation techniques must be practiced by people suffering from COPD as it helps control associated stress and anxiety. Anxiety and panic attacks worsen the breathing in an otherwise healthy person, so these can severely affect a person with COPD. Mediation and yoga can also help reduce anxiety and calm the mind.
- Black Tea: Black tea is rich in tannins and other substances that boost immunity. Black tea reduces the inflammation of the lung airways and inhibits the infection. It helps a person with COPD to breathe properly by decongesting airways. Around 3-4 cups of green tea can be consumed in a day.
- Garlic: Garlic is well known for its anti-inflammatory and antimicrobial properties. It reduces infections in the lung airways, clears the phlegm and eases breathing. Add honey to the juice of garlic and consume this mixture thrice daily.
- Black Pepper: Black pepper clears and eliminates mucus from the lung airways. Crush a few peppercorns and add honey. Consume this paste in the morning for best results.

Health Tip by Expert
It is very crucial to quit smoking after a person has been diagnosed with COPD. Quitting to smoke would help prevent worsening of COPD symptoms. If a person is unable to quit even after several attempts, he/she must join a smoke cessation program.





