Tuberculosis (TB)- A disease with no boundaries has a long history of being dreaded and despised by everyone from common people to public health professionals, doctors and even political parties.
“Tuberculosis” and “epidemic” go hand-in-hand. Owing to the air-borne nature of its infective organism, tuberculosis has claimed millions of lives in the past and is still doing so. As per a recent estimate by Center for Disease Control and Prevention, 1.7 million deaths were reported worldwide due to TB in 2016. [1]
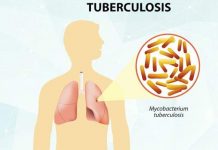
Mycobacterium tuberculosis, the bacterium that causes TB, can affect any part of the body, but most commonly affects the lungs. One of the many reasons TB is dreaded so much is that it doesn’t limit itself to one person. When an infected individual sneezes or coughs, the bacteria are propelled into the surrounding air. Inhaling just a few of these bacteria is enough to infect a person who is in the vicinity. This capacity to infect a large number of people at a time led to wipe out of several families and even small civilizations in the past.
Another feature that makes this disease deadly is the ability of TB bacteria to stay dormant or inactive in people for a long duration of time, medically known as Latent TB. However, such individuals are not considered “infective” as they don’t have any symptom of the disease and cannot transmit the disease to others. The immune cells keep a check on these bacteria, and if the immune system gets compromised in these people, the bacteria may become active and cause a full-fledged infection.
A certain group of people is always at a greater risk of acquiring the disease. The pioneer in these high-risk groups are immunocompromised individuals, i.e., people with low immunity, including people suffering from HIV, cancer, diabetes, smokers, etc. Of these, HIV is of prime significance as most of HIV patients succumb to death every year on developing TB. As per WHO’s statistics, 1 million HIV infected people developed TB in 2016, of which 0.4 million died due to the co-morbidity. [2] Other people at high risk of facing the brunt of TB include children, elderly and residents of developing countries.
Origin of Tuberculosis Infection

Ever thought, where did TB originate from? Who bought this horrendous disease in the world? If you think this disease showed its first mark in the 21st century, you may be taken aback by the fact that traces of this infection date back to as ancient as the era of Egyptian mummies. Some eminent researchers of the world have been studying the genome of animals and humans from different parts of the world, to locate the exact origin of the disease. With the extensive research still being in its active stage, several theories regarding the origin of TB have been proposed. One such research paper published in the Journal of Preventive Medicine and Hygiene, gives a comprehensive historical view of the disease. [3]
The research study lays down an interesting fact, that earliest evidence of tuberculosis was seen in Egyptian mummies dated 2400 and 3000 BC. In fact, historical probing has also revealed that even in 1500 BC, Egypt had hospitals for treating TB. No wonder, scientists consider TB to be the first disease known to mankind.
Some scientists believe that TB originated in South Africa in a particular period, known as Neolithic transition, around 10,000 years back when humans were domesticating animals and indulged in farming. Researchers put forward a theory that animals were infected with tuberculosis bacteria, which was then transmitted to humans.
However, recent research has shown that TB did originate in Africa, but not in animals but in humans itself. Scientists believe that humans acquired the infection first, which was then passed on to the domesticated animals, like cows and goats. This infection was further transmitted to seals which came up on African land for breeding. The infected seals then carried the infection from Africa, across the Atlantic, to reach other parts of the world. Hunters of these animals acquired TB and spread it to other humans. Isn’t it strangely interesting to think that one seal created the whole havoc.
History of its Diagnostic and Treatment Advances
While the origin of TB may have intrigued you, its treatment approaches and the social dogma associated with it, may startle you. With passing centuries, TB was being addressed by several names, including “consumption”, “phthisis”, “scrofula”, “pott’s disease” and “white plague”. In the ancient era, fresh air, milk and rest were considered the only treatment of the disease.
The middle age marked the onset of an interesting era of the disease. In 12th century, people of France and England believed that a royal touch is the cure of TB, i.e., infected people visited royal tombs to seek treatment for their ailment. This justifies the name people gave it, “King’s evil”.
18th and 19th century came with poor sanitation, increase in population density, malnutrition, overcrowded living conditions and several other factors that favored the growth of tuberculosis bacteria. These centuries saw an alarming number of deaths due to TB, thus calling the disease “the robber of youth” and “captain of all these men of death”. This disease claimed lives of so many young and middle-aged individuals, that people’s feelings outweighed their reason when referring to the disease as “romantic disease”.
The term “tuberculosis” was finally coined in the mid-19th century by Johan Lukas Schonlein. Scientists of this era struggled to decipher the illness. Some thought of it to be genetic, while some related it to demonic impact. A German physician thought that TB was caused by an inability of heart to pump blood to lungs. So, he suggested that people suffering from the illness should reside in sanatoriums, which were isolated places, well above the sea level, where heart functions better.
Finally, Robert Koch was able to isolate the bacteria and was able to present to the world the causative organism of TB. He presented his achievement to Physiological Society of Berlin, on 24th March 1882. Since then, this day is celebrated as “World’s Tuberculosis Day” to commemorate his outstanding contribution to the medical field. The concept of sanatoriums and all other absurd theories were completely shunned when Koch demonstrated the infective nature of the disease.
Center for Disease Control and Prevention, further gives an insight on how the treatment approaches of TB changed with time. Striving to find the cure, Koch came up with role of “tuberculin” in 1890. [4] According to him, proteins derived from TB bacteria, which he called tuberculin, can cure the disease. His suggestion was nullified. However, later the concept of tuberculin was considered significant. Skin tuberculin test is still used as a useful method to diagnose TB.
1910 marked the death of an ardent scientist, Robert Koch. He left the world with his remarkable work on diseases like, TB, anthrax, cholera and trypanosomiasis.
With progressing centuries, TB was seen to encroach people of all age, gender, race and socio-economic status. This prompted the need for a definitive cure. Several methods were suggested and rejected in the 20th century. One such method was known as pneumothorax procedure. It involved surgically collapsing the infected lung and allowing it to heal. However, this method was found ineffective.
With further advancements, a drop in the cases of TB was seen following the invention of a vaccine in 1921, called BCG (Bacillus-Calmette-Guerin) vaccine, that claimed to prevent the onset of TB. However, its efficacy in adults is controversial and is hence used in limited countries.
This was followed by discovery of certain drugs, which can act against TB bacteria. First of these to be discovered was streptomycin in 1943. A year after the invention of streptomycin, a patient received the drug and got complete remission from the disease, or at least the scientists thought so. With losing so many loved ones, people looked at this drug to be as the long-awaited magic potion to their demise. But, was it really eligible to be called as “magical drug” for TB. No, it wasn’t.
Emergence of Drug-Resistant Tuberculosis
The New England Journal of Medicine lays down several failures encountered by the treatment advances of TB. [5] 1948 marked the first large-scale clinical trial of streptomycin, conducted by British Medical Research Council. The trial concluded with a mixed response, showing some patients to be completely cured, while some having developed relapse of the infection. On further investigation, it was seen that a large proportion of these patients demonstrated TB bacteria, which had developed resistance to streptomycin. This was referred to as “Drug-Resistant Tuberculosis”.
This was followed by discovery of other drugs, including isoniazid in 1951, pyrazinamide and cycloserine in 1952, ethionamide in 1956, rifampin in 1957 and ethambutol in 1962. But, resistance to these drugs generated a wave of hopelessness among the researchers and general population.
With epidemics of the drug-resistant variant of the disease, came a huge burden on global economy to eradicate it. To top it, the outbreaks of the disease were more common in poor countries. At this critical time, WHO was supposed to take a definitive action. Instead, it stated that deadly diseases like TB and leprosy, require a vigorous drug therapy and an on-going care, thus making these diseases “cost-ineffective”. But, looking at the growing prevalence of drug-resistant TB, World Bank took the initiative to declare that a combination of drug therapy can prove cost-effective in the treatment of TB. WHO seized the opportunity and came up with something known as DOTS (Direct Observation Treatment Strategy). This strategy clearly outlined that the diagnosis of TB should be carried out using smear microscopy alone and treatment of TB should be done with first-line medications (i.e., isoniazid, rifampin, streptomycin, pyrazinamide and ethambutol). An exceptional feature of DOTS was that ill patients were kept under observations to ensure their adherence to drug regimen.
Emergence of Multi-drug Resistant Tuberculosis (MDR-TB)

With the introduction of multi-drug chemotherapy, people, government and researchers thought to have found the treatment they all longed for quite a considerable time. However, soon after the discovery of DOTS, late 1990s saw the advent of a horrid clinical scenario, i.e., “Multi-Drug Resistant Tuberculosis”, commonly called as MDR-TB. WHO defines MDR-TB as a TB showing resistance to at least Isoniazid and Rifampin, with or without resistance to other anti-tubercular drugs. [6]
Epidemics of MDR-TB shook everyone, in particular, political parties and WHO, who had recently started taking pride in coming out with DOTS therapy. This challenged not just the treatment approach, but also questioned the specificity of smear microscopy diagnostic test. With this came a set of remarkable inventions in recognition and treatment of TB.
The importance of chest X-ray, sputum test and Skin tuberculin test cannot be underestimated, but these tests do not precisely locate the drug-resistant strains, thus proving inadequate in case of MDR-TB. This prompted the researchers to develop a Drug Susceptibility Test (DST) to identify and effectively treat MDR-TB. With the emergence of resistance to multiple drugs in TB bacteria, came the discovery of another group of drugs, known as second-line anti-tubercular drugs. These include oral and injectable drugs, mostly belonging to specific drug classes, called fluoroquinolones and aminoglycosides.
Emergence of Extensively Drug-resistant Tuberculosis
The resistance of TB bacteria did not reach a halt even with such diagnostic and treatment advances. In 2006, first case of another variant of TB was reported, known as “Extensively Drug-resistant Tuberculosis”, also known as XDR-TB. WHO defines this particular variant as tuberculous strain, demonstrating resistance to at least isoniazid and rifampin, along with resistance to fluoroquinolone and at least one out of the three second-line injectable drug (i.e., kanamycin, amikacin and capreomycin).
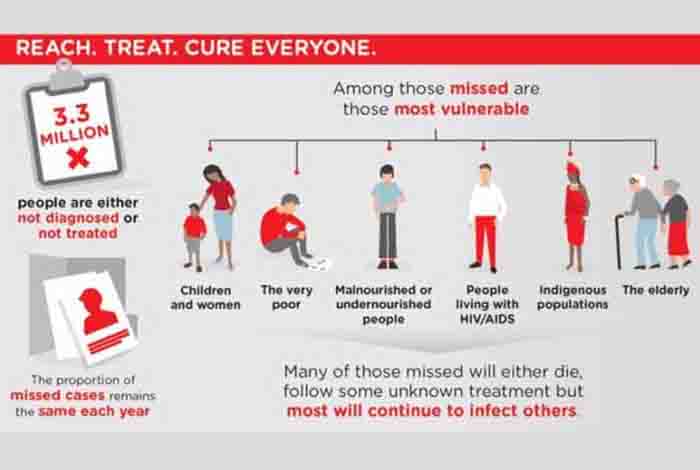
MDR-TB and XDR-TB have caused and are still causing loss of several lives. A research paper published in the Journal of Thoracic Disease outlines the estimate by WHO, stating that as per a 2015 report, of the 4,80,000 cases of MDR-TB, only about 25 percent were detected and less than 50 percent were cured. [7]
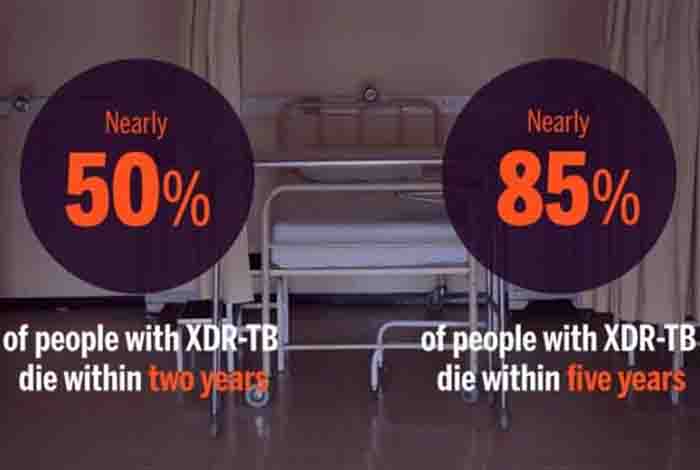
The newly emerged XDR-TB is considered extremely fatal. As per a TB alliance annual report, almost 40,000 XDR-TB cases are spread across 105 countries. The worst part of the disease is survival rate, which is only 15%, less than some severe diseases like Ebola (50% survival rate). [8]
Emergence of Totally Drug-resistant Tuberculosis

Just when researchers were beginning to tackle the XDR-TB, a new variant of TB was developing whose resistance expanded further to involve some more drugs. How far has the resistance expanded, Is the first question that comes to the mind. As per a recent study published in the International Journal of Clinical and Experimental Medicine, a new variant of tuberculosis has been identified in South Africa, which is resistant to all the first line and second line drugs of TB. Although WHO has not recognized this disease yet, few literatures have referred to this disease as “Totally Drug-resistant Tuberculosis” and some also call it “Extremely Drug-resistant Tuberculosis” or XXDR-TB. Offering an extremely questionable outlook, Center for Disease Control and Prevention has called the disease “virtually untreatable”. [9].
Science Behind the Drug Resistance
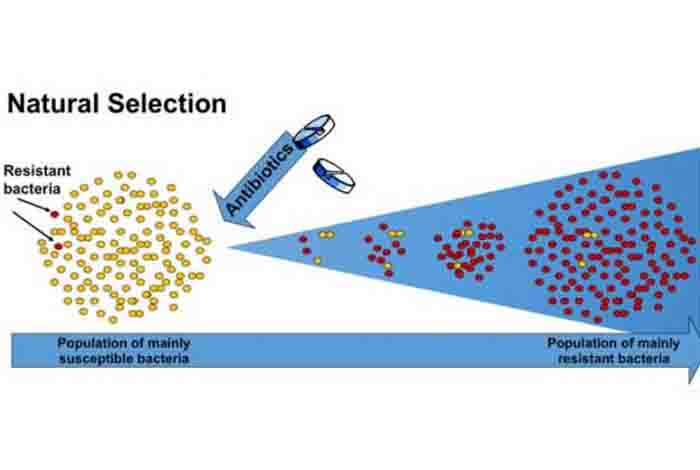
Generating awareness about the drug resistance of diseases and imparting knowledge about what leads to development of drug resistance in bacteria is very important to curb the growing menace of this disease. So what causes disease resistance in TB bacteria Well, several reasons have been attributed to it. Mutation of the genetic makeup of bacteria is the chief factor.
Incomplete or inappropriate treatment and inconsistency in taking medication from the patient’s end can produce drug-resistant strains. This is so because when your doctor does not investigate further to know the drug susceptibility of the infection, the treatment offered by him/her may not kill the TB bacteria effectively, instead make them resistant to the drugs
Steps Taken in Fight Against Tuberculosis
Isn’t it apt to say that TB strains have left human far behind in evolution. They are evolving at a much faster pace than us. There is no denying the fact that looking at the entire clinical scenario of TB, soon history will repeat itself. If not controlled now, TB will produce epidemics with high death rates even higher than the most dangerous cancers such as breast cancer or prostate cancer.
As one would usually expect, MDR-TB drug therapy needs to be taken for years to eradicate all the infectious agent. Well, WHO has come up with some new recommendations, including a short regimen for resistant TB, lasting for 9 to 12 months only. It also offers other advantages like being less expensive and more effective.
WHO also enlists the following points in counteracting the resistant TB infection. [10]
• Eliminate TB infection, as and when identified, in the first time only
• Diagnostic approaches should be easily accessible to all, as many cases go undetected every year.
• A strict infection-free environment should be maintained in areas where TB patients are being treated
• Second-line drugs should be incorporated in the regimen appropriately
What is the Outlook?
Although WHO and other eminent bodies have been working to their full potential to combat the condition effectively, it cannot be completely stated that TB is no longer a threat to the world. In fact, with the pace at which Mycobacterium tuberculosis is evolving, it necessitates a more focused approach. While MDR-TB and XDR-TB are still being worked upon, TDR-TB has not reached anywhere near a complete remission.
An ample funding of the research activities in this domain, along with increased awareness about the disease can help prevent this epidemic to wipe out our civilization in the nearing future.