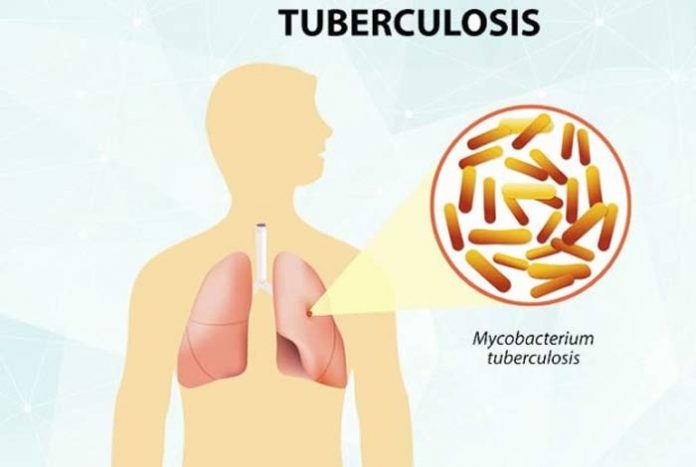
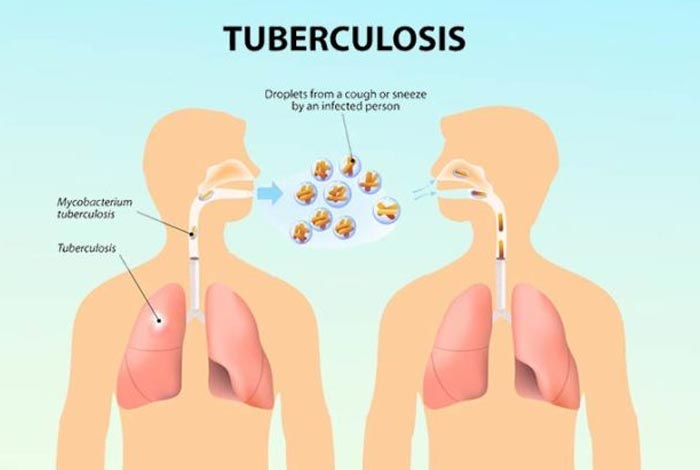
Tuberculosis or TB has been a leading infectious disease that has plagued humankind since the Neolithic times. It is a disease that usually attacks the lungs but can spread to other parts of the body as well, like spine, brain, lymph, bones and joints. It is caused by a bacteria Mycobacterium tuberculosis which is spread through air. When an infected person sneezes, coughs, laughs, talks or sings, tiny droplets laden with bacteria are dispersed in the atmosphere surrounding him, which if inhaled by a healthy person can cause infection. Although TB is an infectious disease, it is not easy to catch. The bacteria grow extremely slowly in the body and a considerably high amount of exposure is required. The bacteria do not thrive on non-living surfaces and therefore, you cannot develop TB by sharing food and water or shaking hands with an infected person.
This deadly disease has been known by various names like scrofula, phthisis, consumption, Pott’s disease and the White Plague. It has been present on earth for more than 6000 years and is hypothesized to have originated in Africa. When humans started migrating from the African continent, they carried tuberculosis with them. During 17th and 18th centuries, tuberculosis accounted for nearly 25% of the total deaths. History was created in 1882 when Dr. Robert Koch discovered the causative bacteria of tuberculosis and paved the way for better treatment of this disease. To mark the importance of this discovery, March 24th is celebrated as Tuberculosis Day throughout the world in order to raise awareness about the devastating health, economic and social consequences of TB and to escalate the efforts for global eradication of the disease.
Despite the continuous efforts by various agencies of world, TB continues to claim nearly 4500 lives every day worldwide.[1] One of the major hindrances in eradicating this ancient disease is the bacterium’s ability to go into a latent stage where it does not produce any symptoms and goes undetected for decades. A more recent development in this bacterium is the emergence of multi-drug resistant tuberculosis (MDR TB) and extensively drug-resistant tuberculosis (XDR TB), which do not respond to the common drugs prescribed for treating TB. These newer strains have developed due to the following reasons:
- Non-compliance of complete course of treatment
- Prescribing wrong treatment, dose for wrong lengths of time
- Unavailability of drugs
- Availability of drugs of poor quality
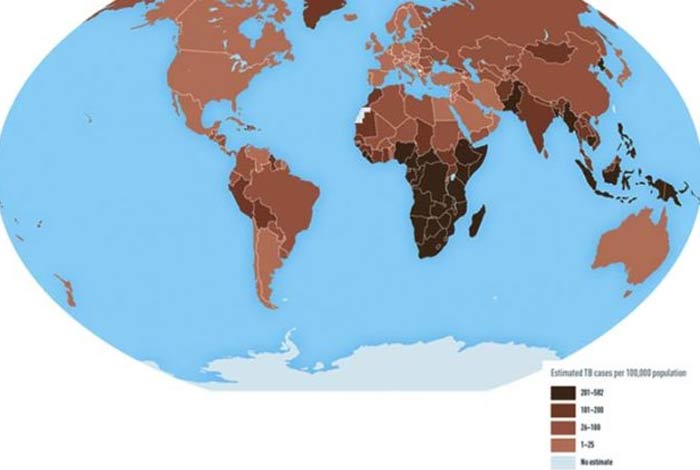
Approximately 10.4 million people fell prey to TB, which claimed the lives of 1.7 million lives globally, out of which over 95% occurred in low- and middle-income group countries. India leads the world with maximum number of TB patients in the country, followed by Indonesia, China, Philippines, Pakistan, Nigeria and South Africa. These 7 countries account for nearly 64% of the total cases of TB of the world. In 2016, nearly 40% of people with HIV infection died from TB. Multidrug-resistant tuberculosis (MDR TB) is the new public health crisis that has emerged in the recent times and has posed an extensive threat to the health and well-being of people across the globe. Through combined efforts of various health agencies throughout the world, the incidence of TB is coming down at a rate of 2% per annum, which needs to be accelerated to 4-5% if we wish to reach our 2020 milestones of the END TB Strategy. The global aim of ending the TB epidemic by 2030 is one of the health targets of the Sustainable Development Goals of WHO. [2]
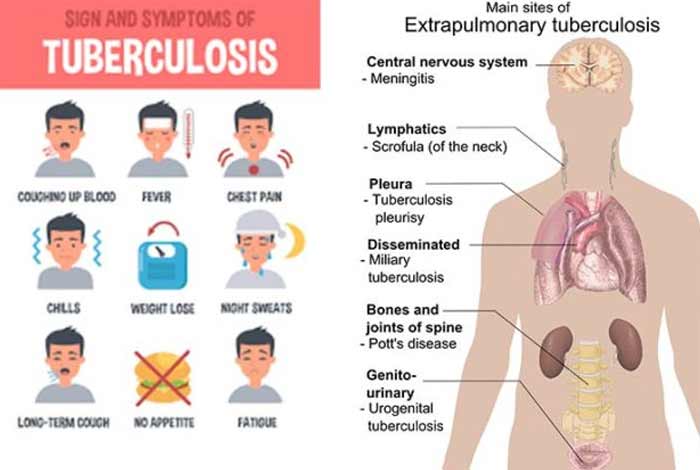
Types and Symptoms of Tuberculosis
Tuberculosis generally affects the lungs but, in some cases, can affect other organs and tissues as well. When a person is exposed to the tuberculosis bacteria, it undergoes three stages, namely:
1. Primary stage
2. Latent Stage
3. Active disease
In the primary stage, there is infection in the lungs after an exposure to TB bacteria. Most of the people recover from it.
The disease gets into the latent stage when there are no symptoms of the disease. The infected person does not feel sick. It is because the immune system is protecting the body and not allowing the bacteria to develop an infection.
People who have latent form of TB cannot spread infection to others as they are non-infectious.
Without treatment, nearly 5-10% cases go on to develop into active TB in the later stages. About half of the people infected with TB bacteria develop the active form of disease within the first two years of exposure.
Some of the characteristics observed in a person with latent TB are:
- Positive skin or blood test for TB
- Normal chest X-rays and negative sputum test
- Does not feel sick
- Is non-contagious
- Is in need for TB treatment to prevent it from developing into active form of disease
In the active stage of the disease, the TB bacteria defeat the immune system and start multiplying in the body. There is a shift in the status of the disease form latent to active. Some people might directly develop active TB, while others develop later. People who have active form of disease are contagious and can spread the disease to others. If TB is suspected, immediate medical intervention should be done and proper and complete treatment should be taken by the person. It should be noted that TB is a serious disease and can become fatal if not treated properly.
The TB bacteria generally affect lungs but can affect other organs and tissues as well. Following are the different types of tuberculosis:
1. Pulmonary Tuberculosis
It is the most common form of TB which occurs when the TB bacteria, also called tubercule bacteria, make lungs as their holy abode. Early diagnosis and proper and complete treatment with antibiotics can treat the infection completely. It is a highly contagious disease and therefore, caretakers need to follow proper precautions for protecting themselves from catching the infection themselves. It can spread through coughing, sneezing, singing and laughing. The droplets containing the bacteria get suspended in the air and can remain there for a long period of time. If a healthy person inhales these droplets, he might get infected and develop TB. However, it requires an extremely high exposure for a prolonged period of time in order to contract TB.
Symptoms observed in pulmonary tuberculosis are:
- Continuous coughing
- Blood in sputum
- Consistent fever, generally low-grade fever
- Night sweats
- Chest pains
- Unexplained weight loss
- Fatigue
2. Primary Tuberculosis Pneumonia
This is an uncommon type of TB that presents itself as pneumonia but is extremely infectious. It is more commonly found in extremely young children, elderly, and people with immunocompromised situations like those on long-term corticosteroid therapy or HIV/AIDS patients.
3.Tuberculosis Pleurisy
Pleural space refers to a space between the lungs and the chest wall, which has a small amount of fluid present in it. Soon after the initial infection with tubercule bacteria, the amount of fluid in the pleural space increases dramatically, which compresses the lungs and produces a number of classical symptoms like sharp chest pain that hinders deep breath and shortness of breath. Significant amount of fluid can be detected in the chest X-ray. The symptoms are accompanied wbymild- or low-grade fever. Tuberculosis pleurisy generally resolves on its own and requires no treatment. However, in about 2/3rd of patients, it might develop into active pulmonary TB within a span of 5 years.
4. Cavitary TB
It is a highly contagious form of TB which involves the upper lobes of the lungs. There is progressive lung destruction by the bacteria through formation of cavities or enlarged air spaces. It is generally seen when the disease becomes reactive after being latent for a long period of time. It generally affects the upper lobes of the lungs because they are highly oxygenated and provide an environment in which the bacteria thrive. Cavitary TB is rarely seen after a primary infection. Occasionally, the disease can spread to the pleural space between the lungs and the chest cavity, cause pus and result in TB emphysema.
Productive cough, fever, night sweats, weakness and weight loss are some the symptoms commonly observed in patients with cavitary TB. Hemoptysis or coughing of blood might also be observed in some cases.
5. Miliary TB
It is a rare form of active TB in which the bacteria find their way to the bloodstream and spreads all over the body. It affects multiple organs and forms tiny nodules in the infected organs. Chest X-rays show the presence of millet seeds-like small nodules all over the lungs. It can become life threatening in a very short period of time. The patients develop high fever and become seriously ill in a very short time. There is a chance that the disease might progress to chronic illness and cause slow decline.
It is difficult to diagnose miliary TB because the initial chest X-rays are clear. Within a short span of time, fever, weight loss, night sweats and other characteristic symptoms develop. It is commonly found in children and immunocompromised people who are exposed to the infection.
6. Laryngeal TB
An extremely infectious form of TB that can infect the larynx or the vocal cords of the person is called laryngeal TB. It is a rare disease which presents itself with hoarseness of voice and dysphagia along with other nonspecific symptoms. This type of TB mimics malignancy in various ways. Biopsy is the only way to confirm it, which is a major hindrance in the accurate and timely diagnosis of the disease.
7. Extrapulmonary Tuberculosis (EPTB)
It constitutes nearly 20% of all the cases of TB reported. EPTB affects organs other than lungs, like lymph nodes, skin, bones and joints, meninges, abdomen, pleura and genitourinary tract. There is a possibility that a person might develop both pulmonary and extrapulmonary TB and is classified as a case of pulmonary TB. [3]
It is difficult to diagnose EPTB because the sites at which TB develops is inaccessible and the tests available are not sensitive enough to correctly diagnose it.
It is generally seen in immunocompromised patients.
Types and Symptoms of EPTB:
a. Lymph Node TB
Lymph nodes are the hub of macrophages, the soldiers of our immune system. Macrophages detect, capture and engulf the bacteria. In people with compromised immune system, macrophages are lesser in number and therefore, if bacteria enter the body, they can make lymph node their home and multiply there. This can make the lymph nodes inflamed and lead to a condition known as lymphadenitis.
In case of TB lymphadenitis, also known as scrofula or King’s evil, when the lymph nodes get inflamed due to TB bacteria, no general symptoms of TB are observed. It is more commonly observed in children and women. Often, lymph nodes on both sides of neck and sometimes those of abdomen are involved.
It is sometimes difficult to manage TB of lymph nodes but most of the cases are generally managed through medication and surgery is rarely required.
In the initial stages of the disease, the lymph nodes are firm, mobile and discrete. With time, they become inflamed and in advanced cases, there might be formation of sinus tracts and abscesses, which might or might not ooze out pus containing TB bacteria.
b. Tuberculosis Peritonitis
It is a serious form of tuberculosis, involving the peritoneum, which is a membrane lining the abdominal cavity. This type of TB is especially common in people who have liver cirrhosis or chronic kidney disease or otherwise a weak immune system. A chest X-ray might show some old evidence of pulmonary tuberculosis but that is generally insignificant. However, better results can be obtained by using CT scan and ultrasound. [4]
There are 3 types of tuberculosis peritonitis, namely wet type, fixed fibrotic form and dry or plastic form. There is an increase in the production of fluid between these layers, which causes pain and abdominal distention.
c. Tuberculosis Pericarditis
Pericardium is the membrane surrounding the heart. It can become affected by TB bacteria and cause tuberculosis pericarditis. The space between the pericardium and the heart begins to fill up with fluid, which impairs the heart’s ability to fill with blood and beat efficiently.
d. Osteal Tuberculosis (H3)
The TB bacteria can travel through the bloodstream, reach the bones and infect them. One of the most common sites for the TB bacteria to take shelter and infect are the spine and weight bearing bones. Infection in the spine can lead to deformity of the back and compression fractures. If it is left untreated, the infection can spread from one spine to the other while destroying the spinal discs in between them. In severe cases, the spine can collapse completely, causing paralysis.
e. Renal Tuberculosis
It is a type oTB that affects the kidneys, one or both. The inner part of the kidney, called medulla, is most commonly affected, although the infection starts from the outer part, called cortex. After the primary infection in the lungs with tubercule bacteria, kidneys can develop tuberculosis after 5-25 years. In some cases, primary renal tuberculosis can also occur in which the tuberculosis develops first in the kidneys. Such a situation occurs when the BCG vaccine, meant for providing immunity against TB is directly introduced in the bladder.
Blood in urine, reduced kidney functions, presence of pus or protein in urine and increased urine frequency along with fever, productive cough and night sweats are some of the commonly observed symptoms of renal tuberculosis.
f. Adrenal Tuberculosis
TB bacteria infecting the adrenal gland can cause tuberculosis of adrenal gland due to which the body is unable to meet the demands of stress hormone at times of need, leading to weakness and collapse. This situation is called adrenal insufficiency.
The symptoms produced in adrenal tuberculosis are nonspecific and are often ignored till it becomes severe or the body is unable to perform under a stressful situation.
g. TB Meningitis
Meninges are the main membrane that surround the brain and the spinal cord. When this membrane gets infected with TB bacteria, it can be life threatening for the person. Even if the person recovers from the infection, the disease can cause permanent impairment in the body, which can be devastating for the person.
It is difficult to distinguish TB from brain tumor because both present themselves as a focal mass in the brain accompanied by neurological symptoms. There is also a danger of patient undergoing stroke. The cardinal features of the disease are headache and fever, with confusion occurring in later stages. Focal neurological defects like vision, speech and hearing problems can also be seen.
Causes of Tuberculosis
The causative organism of tuberculosis is a bacterium called Mycobacterium tuberculosis. It spreads from one person to other when a person with active disease sneezes, coughs, laughs or sings and leaves behind thousands of droplets laden with the bacteria in the air. These droplets can remain suspended in the air and when inhaled by a healthy person, can cause TB. However, it should be noted that a sufficient quantity of exposure is required in order to develop the disease.
Although the mode of transmission of TB is similar to that of flu or common cold but it is less contagious. People with extra-pulmonary TB are less contagious.
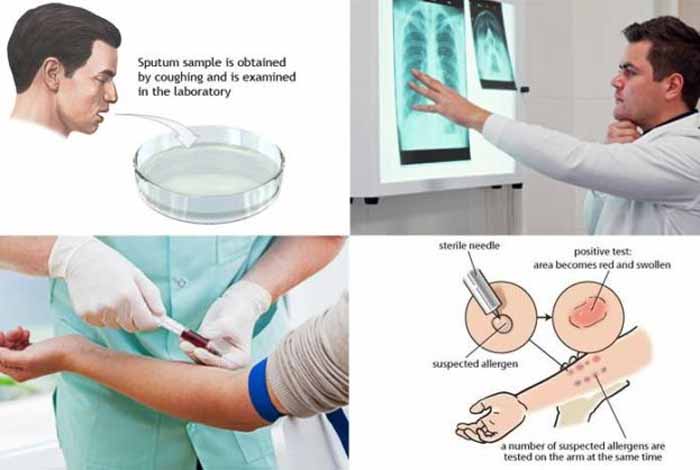
 Diagnosis and Tests of Tuberculosis
Diagnosis and Tests of Tuberculosis
If it is suspected that a person has TB, the general practitioner will conduct an extensive examination.
a. Physical Examination
A thorough physical exam is done where the lymph nodes of the person are evaluated for any kind of swelling and lung sounds are checked. Complete medical history of the patient is taken in order to assess the patient’s risks of developing the disease.
b. Montoux Test
Most common tests for diagnosing TB is a simple skin test, also called Mantoux test or tuberculin skin test (TST), although blood tests are also gaining popularity. A substance called PPD tuberculin is injected just below the skin on the inner side of the patient’s forearm. The health care evaluator then checks the site of injection after 48-72 hours for any type of swelling. If a hard, red, raised bump is observed at the injection site, it is most likely that the patient has TB. Bump size is used to determine the significance of the results.
This skin test can sometimes give false positive or negative test results. If the person has been recently vaccinated with BCG vaccine for providing immunity against TB, then there are chances of getting a positive test result. False negative test results are observed generally in children, elderlies and AIDS patients who do not respond to the skin test. It might be observed in people who have been recently infected with TB but the immune system has not yet reacted to the invasion.
c. Blood Test
Blood tests might be used to confirm the diagnosis of TB or to rule out the possibility of latent or active tuberculosis. Sophisticated technology is used to determine how the patient’s immune system responds to the tubercule bacteria. QuantiFERON-TB Gold in Tube test and T-Spot. TB tests are two such tests that are used for this purpose.
A blood test is useful only when the person is at a higher risk of developing TB, but shows a negative response to the skin test, or has recently been vaccinated with BCG vaccine.
d. Imaging Scans
If a positive skin test result is observed, a chest X-rays or a CT scan might be done in order to determine any changes in the lungs of the patient. These scans also show white spots in the lungs where the immune system walls the bacteria. Better detailed images are obtained from a CT scan.
e. Sputum Test
If chest X-rays display signs of tuberculosis, the doctor might suggest the patient to undergo a sputum test in order to test it for the TB bacteria. Sputum refers to the mucus that is expelled when a person coughs.
Sputum samples also help in determining the strain of the bacteria and determine if it is multi-drug resistant or not. It helps the doctor in determining which medicines are most likely to help the patient.
It can take anywhere between 4-8 weeks to completely diagnose if the person concerned has tuberculosis.
f. Interferon Gamma Release Assay
Interferon gamma release assay (IGRA) is a recent test that is emerging for diagnosing TB. It is useful in diagnosing latent TB if:
- a positive Monteux test is observed
- BCG vaccine has been administered
- an immunosuppressive treatment is to be initiated
If it is suspected that a person has EPTB, additional tests might be performed, such as
Examination of the internal organs of the body using a thin, long and flexible tube which has a light and a camera at its end, called an endoscope. For inserting this endoscope, any natural opening like mouth can be used or, a cut can be made in the skin to insert the endoscope laparoscopically.
Urine and blood tests
Biopsy of the affected area can be done by taking out a small sample of tissue or fluid from it to test it for the TB bacteria.
A lumbar puncture might be performed in which a small sample of cerebrospinal fluid (CSF) is collected from the spine to test it for the presence of tubercule bacteria. CSF refers to the fluid that surrounds the brain.
Treatment of Tuberculosis
Antibiotics are prescribed for several months in order to treat tuberculosis. It can become fatal if proper treatment is not made available to the person, or if the person stops his treatment midway. However, if the complete regimen is followed, deaths are rare. Even hospital care is not required in most of the people.
Directly observed treatment, short course (DOTS), also called TB-DOTS is the control strategy that has been recommended by WHO for controlling TB. DOTS Plus is the control strategy plan for MDR TB.
There are 5 main components of DOTS:
Government commitment (including political will at all levels, and establishment of a centralized and prioritized system of TB monitoring, recording and training)
Case detection through sputum smear microscopy
Standardized treatment regimen directly of six to nine months observed by a healthcare worker or community health worker for at least the first two months
Drug supplies
A standardized recording and reporting system that allows assessment of treatment results
The antibiotics that are prescribed for treating various types of TB are given below:
1. Pulmonary TB
For treating active pulmonary TB, a combination of antibiotics is prescribed for a minimum of 6 months. The usual treatment is:
- two antibiotics (isoniazid and rifampicin) for 6 months
- two additional antibiotics (pyrazinamide and ethambutol) for the first 2 months of the 6-month treatment period
| Preferred Regimen | Alternative Regimen | Alternative Regimen |
| Daily INH. RIF, PZA and EMB for 56 doses (8 weeks) | daily INH, RIF,PZA and EMB for 14 doses (2 weeks), then twice weekly for 12 doses (6 weeks) | Thrice-weekly INH, RIF,PZA and EMB for 24 doses (8 weeks) |
| Continuation Phase Daily INH and RIF for 126 doses (18 weeks) or twice-weekly INH and RIF for 36 doses (18 weeks) |
Continuation Phase Twice-weekly INH and RIF for 36 doses(18 weeks) |
Continuation Phase Thrice weekly INH and RIF for 54 doses (18 weeks) |
Table 1: Basic TB disease Treatment Regimens
Abbreviations: INH: isoniazid, RIF: rifampin, PZA: pyrazinamide, EMB: ethambutol
The treatment might take weeks to finally show improvement in the condition of the patient. The exact length of time will depend on the severity of the condition and the overall health of the patient. After 2 weeks of taking the antibiotics, most people start to feel better and are no longer contagious. However, the most important point here is to complete the entire course of the treatment. This is the junction at which most people make the mistake of discontinuing the treatment and paving the way for multi-drug resistant TB to develop in their bodies. Multi-drug resistant TB is the type of TB which does not respond to the antibiotics generally prescribed for treating TB. It is a potentially serious condition and requires a much longer treatment course with more toxic therapies. The best way to ensure that such a catastrophic situation does not arise is to take the medicines for 6 months.
If proper treatment plan is followed, no further follow ups with a TB specialist are required. A few instructions might be given to look out for any spotting signs in the sputum, which can indicate that the disease has relapsed.
2. Extrapulmonary TB
Same combination of antibiotics can be used for treating EPTB. If the person has TB in the brain or pericardial TB, then corticosteroids might be prescribed along with antibiotics for several weeks in order to reduce the swelling in the affected areas. It is extremely important to complete the full course of the antibiotics and to take the medicines exactly in the manner they are prescribed.
3. Latent TB
When there is an infection with the TB bacteria but no symptoms are observed, that is known as latent TB. If the patient’s age is 65 years or less, then antibiotics can be prescribed. However, in the elderly there is an increased risk of development of liver damage. Treatment is not always prescribed to people with latent infection, especially if multi-drug resistant TB is suspected. In such a case, the patient is regularly monitored for signs of active TB.
In some people, the tests for latent TB might be done before starting the patient on immunosuppressant drugs like corticosteroids for a long-term therapy, biological inhibitors like TNF and chemotherapy. This is done because when the immune system is toned down, these bacteria might become active and cause TB.
Treatment for latent TB generally involves:
either taking a combination of rifampicin and isoniazid for 3 months,
or isoniazid on its own for 6 months
| Drugs | Duration | Interval | Minimum Doses |
| Isoniazid | 9 months | Daily Twice-weekly |
270 76 |
| Isoniazid | 6 months | Daily Twice weekly |
180 52 |
| Isoniazid and Rifapentine | 3 months | Once weekly | 12 |
| Rifampin | 4 months | Daily | 120 |
Table 2: Latent TB infection and Treatment regimes
4. Drug Resistant TB
When this disease is caused by a TB bacteria strain that is resistant to at least one of the first-line-anti-TB drugs, it is called a drug resistant TB. In case of Multi-drug resistant TB (MDR TB), the bacteria are resistant to more than one anti-TB drugs and at least isoniazid (INH) and rifampin (RIF). A rare form of MDR TB is the extensively drug-resistant TB (XDR TB) which shows resistance to isoniazid and rifampin along with any fluoroquinolone and at least one of three injectable second line drugs, kanamycin, amikacin and capreomycin.
Recently, two new drugs namely, bedaquiline and delamanid have been discovered which are showing positive effect in treating drug resistant TB.
It is an extremely daunting task to treat and cure drug resistant TB. Life threatening situations can arise from inappropriate management. It should only be treated by a physician who is an expert in the disease.
 Conclusion
Conclusion
Tuberculosis is an ancient disease that has played an important role in altering world history. Such was the impact of this disease that it even defined fashion in the by-gone years. Being pale and slim, just like a tuberculosis patient, became popular in the Victorian Era. Such was the craze for the disease that having it became the new fashion statement.
When in 1900s, health campaigns started in the U.S. to educate people about the disease, hemlines for women’s dresses and skirts started becoming shorter to prevent them from catching the disease in the street. Beards and mustaches were given away for a clean shaved look as it was though that the bacteria could thrive in the facial hair.
Tuberculosis is also believed to be the main reason behind the invention of pasteurization technique for making the milk germ free, and construction of sanitariums where people could be isolated and treated. It stimulated the research for developing antibiotics as well.
Not only did TB alter the course of history, major world events also affected the mutations of genetic material of the TB bacteria. The fall of USSR is one such event, after which a new strain of virulent and drug resistant TB developed, which continues to plague the people of Central Asia. It spread to Afghanistan and Europe due to population shift and armed conflict.
The world has lost almost a third of its population to this disease and even today, when the medical science has made tremendous progress, TB continues to claim a life every 25 seconds. Although it is a disease that is of concern for the poor nations, it is also a threat for the wealthy countries. When people with latent infection travel to these industrialized countries, they have a potential to spread it among the population there if the disease becomes active.
TB is not a disease to forget. Rather, it requires cumulative effort from all countries of the world to step up and join hands in fight against this disease.