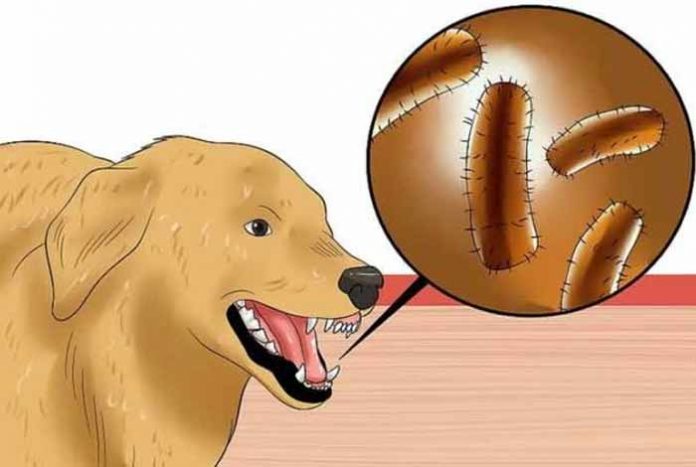
Rabies is a fatal viral disease, which spreads from saliva of infected animals to humans through animal bites or scratches. Although all animals are susceptible to rabies virus infection, few are significant reservoirs of this virus. These infected animals are referred to as “rabid animals”.
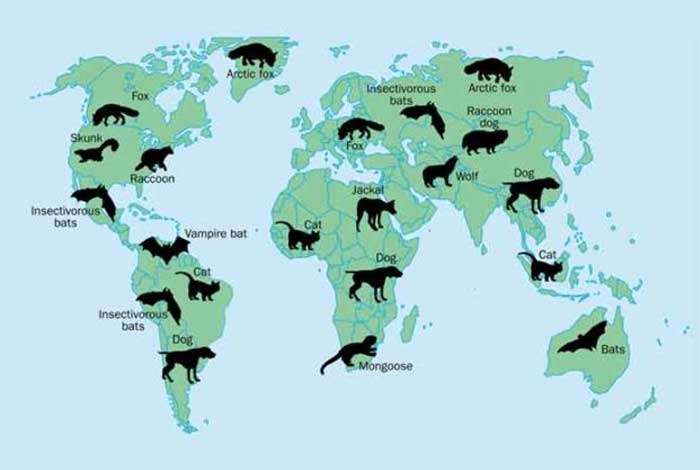
In the US, these include wild animals, like foxes, skunks, raccoons, coyotes and bats. However, in developing countries of Southeast Asia and Africa, stray dogs are the most significant reservoir of rabies virus. Also, it is not uncommon to acquire rabies from pets, including dogs and cats.
Rabies is one of the most common viral disease, seen in more than 150 territories and countries. More than 99% of these cases are caused by an infected dog’s bite. It causes tens of thousands of deaths every year, with more than 95% of cases being reported in Asia and Africa. Children between the ages of 5-14 are the most frequent victims of rabies. [1]
Rabies virus, involves the brain tissue, thus producing symptoms, which are generally mild in the initial stages and become worse with time. If left untreated, it can eventually lead to death.
Rabies is a completely preventable disease. Vaccinating the animals and pre-exposure immunization in humans can prevent this deadly infection. However, if exposed, Post-exposure prophylaxis (PEP) consisting of rabies immunoglobulin can reduce the risk of death due to rabies. Every year, almost 15 million people worldwide receive post-bite vaccination.
Types

Based on the presenting symptoms and the severity of the condition, there are two types of rabies. These are described below.
- Furious Rabies
Also known as classical or encephalitic rabies, this type of rabies produces symptoms such as hyperactivity, restless behavior, and various phobias like hydrophobia (irrational fear of water) or aerophobia (fear of fresh air). This may further progress to cardio-respiratory arrest, leading to death. - Paralytic Rabies
Also known as dumb rabies, this variant is less dramatic but has a longer course than furious rabies. It accounts for 30% of total rabies cases in humans. It usually begins with a flaccid muscle weakness at the site of animal bite or scratch. This weakness then progresses to a gradual paralysis, which eventually causes coma and respiratory failure. Due to less typical symptoms, paralytic rabies is often misdiagnosed, contributing to a significant number of underreported cases of rabies.
Symptoms of Rabies
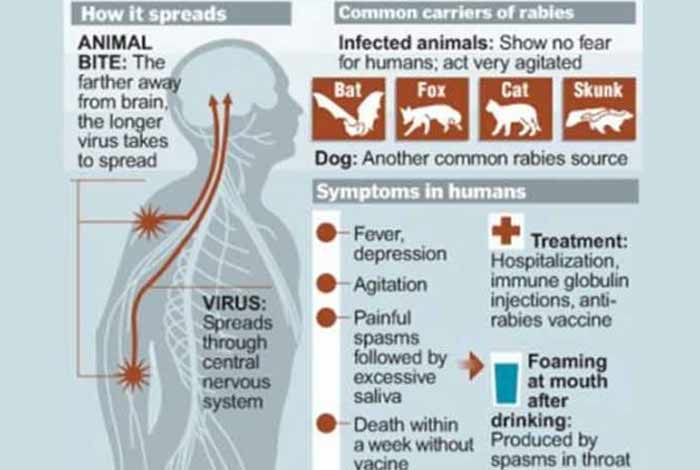
Once rabies virus enters a human body it multiplies and starts showing symptoms. These symptoms can appear as early as after 7 days or maybe as delayed as 1 year. This period is known as incubation period. Typical incubation period of rabies is 2 to 3 months.
As per Centers for Disease Control and Prevention, initially, rabies presents itself as general symptoms of flu, which are described below.[2]
- General discomfort or weakness
- Headache
- Fever
As the disease progresses, it produces symptoms of cerebral dysfunction, such as:
A notable fact here is that, once a person develops these clinical signs, he or she is bound to die due to rabies.
Risk Factors
Certain factors increase the risk of developing rabies. These are described below.
- Developing countries: Due to political neglect, rabies is more common in developing countries, including countries in Southeast Asia and Africa. Living or traveling to these areas can significantly increase the risk of acquiring rabies.
- Activities involving contact with an infected animal: There are certain activities, which involve contact with wild animals infected with rabies. These activities include camping without taking precautions or exploring caves of bat, etc. and can put you at a higher risk of acquiring rabies.
- Laboratory research concerned with rabies virus: A person involved in active laboratory research related to rabies virus, is at a higher risk of acquiring the infection.
- Head or neck wounds: If an infected animal bites in the head or neck region, the chances of dying from rabies increases as the virus travels faster to the brain.
Do I have it?

If you have been bitten by any wild animal or stray dog or a pet, you may have acquired rabies infection. If you have developed clinical signs of rabies (already described above), you have reached a fatal stage of the disease with a very low chance of recovery.
If you have a pet, who has not been vaccinated for rabies, even a scratch by the animal can render you infected. If you woke up with a bat in your room, consider yourself bitten and infected with rabies.
Causes
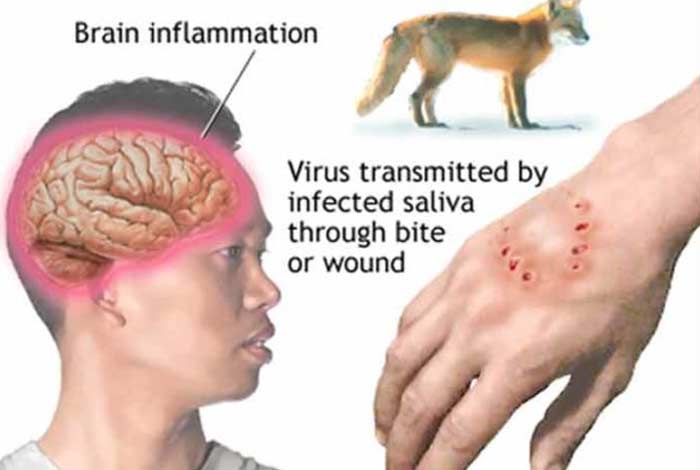
Rabies is a zoonotic disease, i.e., a disease transmitted from animals to humans. This virus is present in the saliva of rabid animals. This virus is transmitted to humans via infiltration into a wound or scratch or by direct exposure of mucous membrane to the virus. A notable fact here is that rabies virus cannot infect an intact skin.
On entering the human body, the rabies virus reaches the brain. In the brain, the virus replicates or multiplies to produce more viruses, thus producing signs and symptoms of infection.
Prevention

Rabies is an absolutely preventable infection. Various methods of prevention of rabies are as follows.
1. Eliminating rabies in rabid animals
Since rabid animals are the reservoir of the virus, vaccinating these animals can significantly reduce the risk of transmission of virus in humans. Therefore, vaccinate your pets and prevent the spread of infection.
2. Keep your pets confined
It is important to keep your pets confined to indoors and supervise them when outdoors. This is so because stray animals and other animals may not be vaccinated against rabies. Exposure of your pet to such animals can infect your pet, which can further infect you and other members of the family.
3. Preventing dog bites and awareness on rabies
Educate the community, including children and adults, about the behavior of dogs and bite prevention. Educate the community about responsible ownership of pets, ways to prevent dog bites and immediate measures after a dog bite.
4. Preventive vaccination in humans
Preventive vaccinations, medically referred to as pre-exposure prophylaxis, must be given to people who are at a high risk of acquiring rabies infection. These include people traveling to rabies-affected areas, laboratory workers with live viruses in the lab and professionals with active contact with wild animals, like animal control staffs and wildlife rangers.
Diagnosis

There is no diagnostic test to determine if the animal bite has transmitted the rabies virus to an individual or not. However, if left untreated, it can progress to development of clinical signs of rabies. The appearance of clinical signs is suggestive of spread of infection to the brain, which eventually leads to death. Therefore, doctors usually treat the individual, considering him/ her infected.
Treatment

As already stated, a person who has been bitten by any animal is considered infected and must be immediately treated. The immediate treatment is referred to as post-exposure prophylaxis (PEP), which includes rabies vaccination and immunoglobulin (i.e., antibodies against rabies virus). Meanwhile, the animal is observed for 10 days to look out for signs of rabies infection. If the animal cannot be captured or if the animal shows signs of infection, full- course prophylaxis is recommended. However, if the animal shows no signs of infection and is proven to be rabies-free, the prophylaxis can be discontinued. Thus, PEP and determining rabies status of the animal form the mainstay of treatment of rabies. These are described in detail below.
1. Post- Exposure Prophylaxis (PEP)
PEP is done immediately after a person has been bitten by an animal. The goal of PEP is to prevent the spread of infection to the brain, thus reducing the risk of death due to rabies.
The key components of PEP are as follows.
- Immediate wound care
Thoroughly flush and wash off the wound for 15 minutes with soap and water, detergent and povidone iodine, or other agents that are capable of killing the rabies virus. - A course of potent rabies vaccine that meets WHO standards
Based on the severity of rabies infection, WHO lays down three categories of individuals. The post-exposure prophylaxis measures vary with each category. These are described below.
| Categories of Contact with Rabid Animal | Recommended PEP Measures |
| Category I: Touching or feeding animal; animal licks the intact skin |
No measure needed |
| Category II: Minor scratches, nibbling of the uncovered skin or abrasions without bleeding |
Local treatment of wound and immediate vaccination |
| Category III: Animal licks on broken skin or mucous membrane, single or multiple skin scratches or bites or contact with bats |
Local treatment of wound, immediate vaccination and rabies immunoglobulin |
2. Determining Rabies Status of Animal
The animal which has bitten the individual should be identified and isolated. The animal is then observed for 10 days to look for signs of rabies infection. The animal may also be euthanized for laboratory evaluation. However, it must be noted that while the animal is being inspected for presence of rabies virus, the individual must continue the post-exposure prophylaxis. However, if the animal is found to be rabies-free, PEP may be discontinued.
Care

Rabies is a deadly virus, causing several deaths every year. Children are most affected by the infection as they are usually unaware of the infective nature of animals and hence, tend to overlook bites and scratches by animals.
Parents must make children aware of rabies and its prevention. Also, child playing with animals must be supervised by parents or other adult family members.
Vaccinating your pet bears utmost importance in preventing the spread of rabies in children and adults. In case of a bite, seek immediate medical help. Also, if you are at a high-risk of getting the infection, opt for a preventive vaccination by a medical professional.
OTC Available
There are no over-the-counter medications available for treatment of rabies. Vaccination by a trained medical professional is the only cure of rabies. Taking any other over-the-counter drug or supplement is strictly condemned. Seek medical help to the earliest in case of bite or scratch by animal or if you lie in the high-risk category of acquiring infection.
Self-Management Methods Available

In case of a bite by an animal, you should manage the condition by the following methods.
1. Wash the wound thoroughly: As already stated, washing the wound thoroughly with soap and water should be the first immediate measure against the infection. Other agents that can be used to kill the virus include povidone-iodine, detergent, etc.
2. Seek medical help immediately: Medical help is a mandate to effectively counteract the rabies virus. Approach a medical professional immediately following an animal bite to prevent the spread of infection to the brain.
Natural Ways to Cure Rabies
Vaccination is the only way to cure rabies. Thus, attempting any natural remedy to combat the infection is not recommended. Seek medical help and get yourself vaccinated to cure rabies.
Health Tip by Experts
Whether you are an animal lover or fond of camping in the wilds, overlooking the fatal nature of rabies infection is not wise. Be a responsible owner and get your pets vaccinated. If suspecting rabies, get a rabies shot and enjoy a rabies-free life with your pet.




