Insulin is a very widely used medicine on which millions of people in this world depend, for managing their diabetes. It is a peptide hormone that is secreted by the pancreas for regulating blood glucose levels.
With the increasing prevalence of diabetes, a disease in which body is unable to regulate blood glucose levels, it is important to know everything about insulin, the form it comes in and how and why should you take it on prescription. So, let’s get started and know all about insulin by answering the following questions:
- What is diabetes?
- What is the use of insulin in diabetes?
- How does it control blood sugar levels?
- What are the non-diabetic uses of insulin
- What is insulin therapy?
- Why Insulin Should be Taken only on Prescription?
- Conclusion
What is insulin?
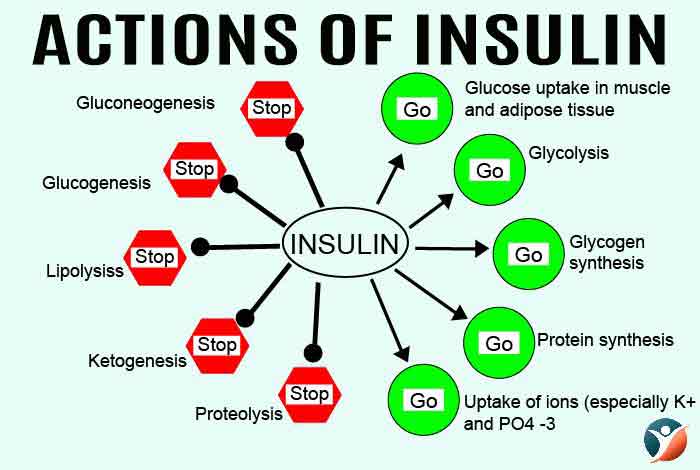
Insulin is a peptide hormone normally made in the pancreas that stimulates the flow of sugar (glucose) from the blood into the cells of the body. Glucose is the food cells take up and convert into energy that is used by us.
From where it comes?
Insulin comes from pancreas, an organ that is a part of the digestive system. Pancreas contains beta cells that are responsible for synthesizing the hormone insulin in response to glucose. Pancreas performs a wide array of functions like controlling blood glucose, digesting proteins and digesting carbohydrates.
It controls blood sugar levels in the body by secreting two hormones insulin and glucagon. Insulin works by reducing the levels of glucose in our bodies while glucagon increases the level of glucose in our body.
Insulin is released in two phases; the first phase begins 5-10 minutes after a surge in glucose levels and the second phase begins after 30-60 minutes.
What is diabetes?
Diabetes is a metabolic disease in which the person has increased levels of glucose in his bloodstream. This result either due to inadequate production of insulin or because the cells of the body do not respond to it, or both. When the body is unable to produce insulin, it is required to supplement it from outside.
What is the use of insulin in diabetes?
Insulin is used in the treatment of people with type 1 diabetes as they are incapable of producing insulin. In case of type 2 diabetes the disease is at first managed by different drugs and if insulin levels remain low despite the use of other types of medications, then insulin is prescribed to these patients also.
Insulin may also be prescribed for patients with gestational diabetes.
How Does Insulin Regulate Blood Glucose Levels?
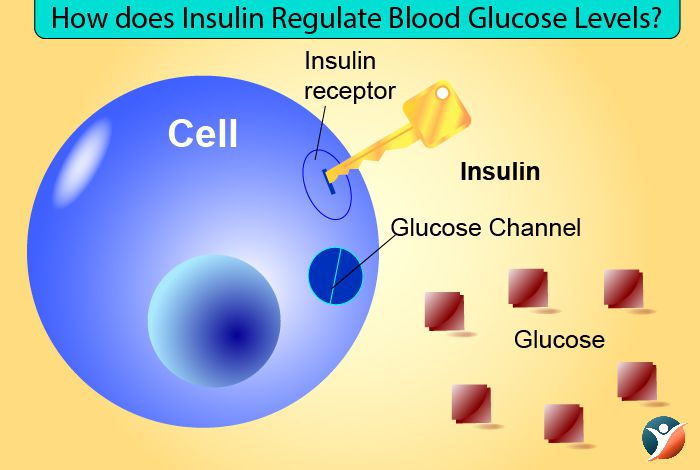
The glucose level in the blood is strictly controlled by insulin. Insulin works to ensure that the production of glucose on digestion is equal to its rate of consumption of by the cells.
In people with diabetes, this balance gets disturbed and the excess glucose is then passed out through urine.
In healthy individuals, insulin ensures that the levels of glucose remain steady in the blood. When the blood glucose level dips, the insulin level also decreases which signals liver to release the stored glucose.
When the glucose level is high in the blood and the insulin levels are also high. High insulin level signals liver to take up glucose for storage in the form of glycogen.
So, the main role of insulin in a healthy body is to signal liver to take up or release glucose in the blood stream.
Cells of the body can take up glucose for energy production in the absence of insulin as well but this is very slow process. Insulin accelerates this process by employing glucose transporter molecules to the cell membrane resulting in a very effective and quick job.
When there is a lack of insulin in the blood stream, the liver keeps on releasing glucose in the bloodstream at a rate that cannot be metabolized by the cells thus leading to diabetes.
What are the non-diabetic uses of insulin?
Insulin is not only used as a drug for diabetes, it is used in many other fields in medicine. Some of these are:
i) Diagnostics: Insulin is used in psychology in Narco-analysis test, in medicine for Insulin Tolerance Test for GH deficiency and as a part of cell growth mediums.
ii) Therapeutic: It is used in weight loss, weight gain and muscle building therapies, in oncology, insulin potentiation therapies are used where insulin is combined with low dose chemo therapy for better results, deep insulin coma therapies and wound healing. Insulin has also been associated with an increased release of Klotho, the anti-aging protein so it is used in anti-aging too.
iii) Surgical: Insulin is frequently used in reducing surgical complications.
What is insulin therapy?

Insulin therapy is an intensive part of treatment for patients whose bodies cannot produce enough insulin. The main aim of insulin therapy is to ensure that the blood glucose levels remain within normal range.
Insulin is generally administered in the fat layer under the skin with the help of syringe, insulin pump or insulin pen. Insulin regimens are tailored as per
i) the needs of the patient,
ii) type of diabetes,
iii) how the glucose level fluctuates during the day
iv) and the patient’s lifestyle.
Different types of insulin available
In the body, insulin is synthesized in the pancreas by the beta cells. It is a hormone that facilitates the uptake of glucose by the cells from blood.
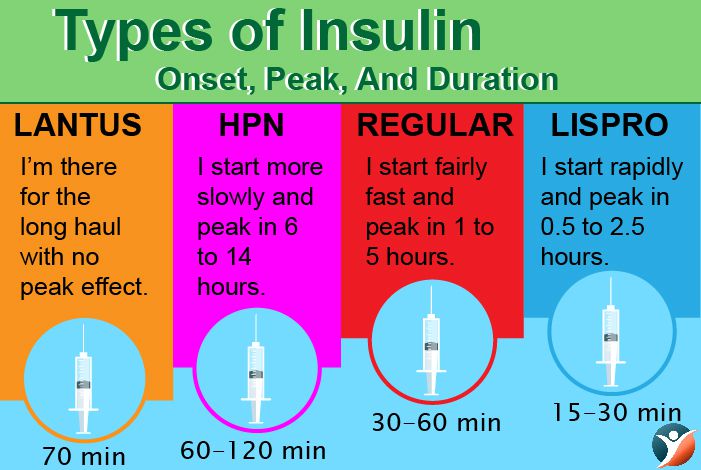
Insulin administered from outside has a similar mechanism of action like the naturally produced hormone. The different types of insulin available in the market differ in the following ways:
- Source of insulin
- Onset time (time taken to start action)
- Peak (time taken to achieve maximum action)
- Duration of action (time for which insulin remains working)
- Route of administration
A. Classification according to onset time and duration of action
1. Rapid Acting Insulin
2.Short Acting Insulin
3. Intermediate Acting Insulin
4. Long acting insulin
1. Rapid Acting Insulin
Rapid acting insulin starts working within 15 minutes of administration and peaks in about 1 hour. It is active for 2 to 4 hours and it is meant to be taken before or with meals. Since, it acts very quickly, produces an increased risk of hypoglycemia. It is administered through injection or insulin pump.
Types of Rapid Acting Insulin:
a. Insulin lispro, Brand name: Humalog
b. Insulin aspart, Brand name: Fiasp
c. Insulin glulisine, Brand names: Apidra
d. Prompt insulin zinc, Brand name: Humulin U
2.Short Acting Insulin:
Also known as regular or neural insulin, it is usually taken before meals.
This group is not as quick as rapid acting insulin. Generally, this group of insulin is obtained from animal or human source.
It is administered via syringe or insulin pen.
It takes between 30 to 60 minutes to start its action and lasts for about 8 hours.
Brand name: Humulin R
3. Intermediate Acting Insulin:
They are often taken along with short acting insulin.
Their action begins 2 to 4 hours after injecting.
It peaks from 4 to 12 hours and works for 12 to 18 hours.
They are also known as isophane or Neutral Protamine Hagedorn (NPH). People taking NPH should be aware of the risk of night time hypoglycemia.
Types of Intermediate Acting Insulin
a. Isophane insulin, Brand names: Humulin 70/30
b. Insulin zinc, Brand names: Humulin L
4. Long acting insulin:
This type of insulin is often used along with rapid or short acting insulin.
It is used for lowering blood glucose level when rapid acting insulin stops.
It is taken once or twice a day.
Available in animal and analogue forms. They can remain active up to 24 hours with the exception of bovine protamine zinc insulin (PZI), which can last up to 36 hours. These do not have any peak activity and has consistent delivery throughout the day.
Types of Long Acting Insulin
a. Extended insulin zinc, Brand names: Ultralente
b. Insulin glargine, Brand name: Lantus
c. Insulin determir, Brand Names: Levemir
B. Classification According to Origin:
1. Animal Insulin: This was the first type of insulin that was administered in humans for managing diabetes and was obtained from cows and pigs. Today, the use of animal insulin has subsided significantly and has been replaced by human insulin and human analogue insulin. However, animal insulin can still be obtained on prescription.
There are 3 different types of animal insulin available, Short Acting, Intermediate Acting and Long Acting Insulin. Premixed animal insulin is prepared by mixing short acting and intermediate acting insulin in different ratios.
2. Human Insulin: It refers to synthetic insulin which is developed in the laboratory and mimics human insulin. It is developed by growing insulin proteins within Escherichia Coli (E.coli). It is of following types:
a. Regular or Short Acting Form
b. Intermediate Acting (Neutral Protamine Hagedorn)
c. Premixed Human Insulin, which is prepared by mixing regular and NPH insulin in different ratios.
3. Genetically Engineered Insulin: This insulin is produced with the help of recombinant genetic technology and is least immunogenic in nature. It is more acceptable to the body and causes less reactions with the immune system. These are genetically altered to create a more rapid acting or more uniformly acting form of the insulin. They are produced by growing insulin proteins inside E.coli and then the sequence of amino acid is changed to increase its speed of action or to make it act more uniformly.
Types:
a. Rapid Acting Insulin : It starts acting immediately after injecting and peaks around 1 hour after injecting. Its duration of action is 4 hours.
Brand Names: Humalog
b. Long Acting Insulin: It starts acting nearly 2 hours after injection and it is expected to work uniformly and hence, has no peak time. Its duration of action is 24 hours.
Brand name: Lantus
c. Premixed: It is prepared by mixing short acting and intermediate acting insulin in different ratios.
Brand Names: Humalog Mix 50
Inhalable Insulin
It is a type of insulin that can be inhaled. It contains powdered form of insulin and can be delivered with the help of a nebulizer directly into the lungs from where it can be absorbed. In general, inhaled insulin is thought to be more rapidly absorbed than the insulin which is injected subcutaneously. It reaches its peak action very quickly and gets metabolized rapidly. It has been approved by the U.S. FDA in 2014.
How to take insulin?
Insulin is administered in the fatty tissue underneath the skin with the help of special insulin syringe. Insulin injections are never given in the muscles. However, if a patient has needle phobia, there are a number of other options by which insulin can be administered. These include:
1. Insulin Pen
Insulin pens can make taking insulin shots extremely easy. These eliminate the need to poke the skin with syringe every time insulin shot is required. These pens can deliver 0.5 to 80 units of insulin at a time.
The maximum dose, incremental values and total amount of insulin units in cartridges vary among pens. The pen comes in two forms, disposable and reusable.
These pens do not require constant refrigeration after being opened. They need to be refrigerated only before the first use. They can remain good to use 7-28 days after initial use, depending on the type of insulin present in the pens.
2. Insulin Pumps
These are small devices, closely resembling a beeper or a miniature computer. Insulin pumps have the following parts:
Reservoir- This is where the insulin is stored. It needs to be refilled regularly to have an uninterrupted supply of insulin.
Cannula- It consists of a small needle and a straw-like tube that is inserted in to the fatty tissue under the skin for administering insulin.
Operating Buttons- These buttons allow programmed delivery of insulin at the site of administration.
Tubing- This is a thin, flexible plastic that carries insulin from pump to the cannula.
An insulin pump is found to be more user friendly and allows the patient to spend an entire day without carrying much of the diabetic supplies. It ensures a more fine-tuned dosing regimen of basal insulin that is less structured around the meal time.
A doctor determines both basal and bolus dose requirements as per the blood glucose levels of the patient throughout the day. A particular glucose level is targeted and the dose is fixed according to it.
Some of the insulin pumps come with the regular monitoring device for keeping a check on the blood glucose level throughout the day. The recent advances in this field is aimed at making these pumps ‘smarter’. For example, in one of the recently developed insulin pump, there is a provision for monitoring the glucose levels and cutting off the supply of insulin when the glucose levels dips too low. The pump is programmed not to resume insulin delivery until the blood glucose levels get back to a particular level.
Another advancement in this field is transferring the blood glucose levels to a computer or recording device that is at a distance of least 50 feet or less. This will allow patients to monitor their kid’s blood glucose levels when they are asleep.
3. Insulin Jet Injectors

Insulin jets are small and complicated devices that deliver insulin without the use of needles. These devices use a compressed spring or gas to deliver insulin on to the skin from where it is then absorbed. Jet injectors that contain compressed gas are more expensive than those containing compressed springs. These injectors have a delivery device that is shaped like a pen, a disposable injector nozzle and a disposable insulin vial adapter. There are tiny openings at the end of the disposable injector nozzle.
Do’s and Don’ts of Insulin Injection
It is the most common method for administering insulin, with the help of a special syringe and needle. The following things should be kept in mind if using insulin injections:
Injections must be given in the subcutaneous tissue.
- A fold of skin should be lightly grasped, and insulin injected at an angle of 90 degree.
- Children and thin individuals must use short needles pinch the skin.
- In thigh area inject at 45 degree in order to avoid intramuscular injection,
a. Mixing Insulin
Sometimes, rapid or short acting insulin is mixed with intermediate or long acting insulin in order to regulate the blood glucose level. Mixed insulin has been found to produce better results than single insulin. However, mixing of insulin should only be done if it is suggested by the doctor because the dosage regimen is customized for each patient. There are a number of factors that affect the stability of mixed insulin like particle aggregation, absorption rate and bioavailability.
b. Syringes
Insulin injections are given with the help of special syringes that are marked in insulin units. The marking on the insulin syringes and their length can vary depending on the manufacturer.
c. Disposal
Recapping, breaking or bending the needle can increases the probability of getting needle-stick injury. These needles should only be disposed as per the guidelines given by local authorities.
e. Needle Reuse
Needles meant for single use should not be reused as they are designed in such a way that their shape gets distorted after the use. If such a distorted needle is used again, it can increase the chances of needle-related injuries. Multiple use of a single needle can also help in spreading infections.
If needle reuse is the only option left, then precautions must be taken for maintaining its required sterility and safety. Reused syringe can be kept at room temperature as the risks or benefits of refrigerating needles is not properly understood. Wiping needle surface with alcohol should be avoided to prevent erosion of the silicon coating of the needle which can make skin puncture procedure a more painful experience.
g. Dose Preparation
Before preparing a dose, the label of the insulin bottle should be read carefully in order to avoid injecting an incorrect dose of insulin. The injection site and hands should be clean. The vial is to be rubbed gently between the palms of the hands in order to re-suspend the insulin. After drawing insulin into the syringe, the fluid should be checked for air bubbles.
Air bubbles are not dangerous in themselves but can decrease the injected dose. After preparing the dose, it should be checked whether the prepared dose is cloudy or not. Only clear solution should be injected.
Injection Sites
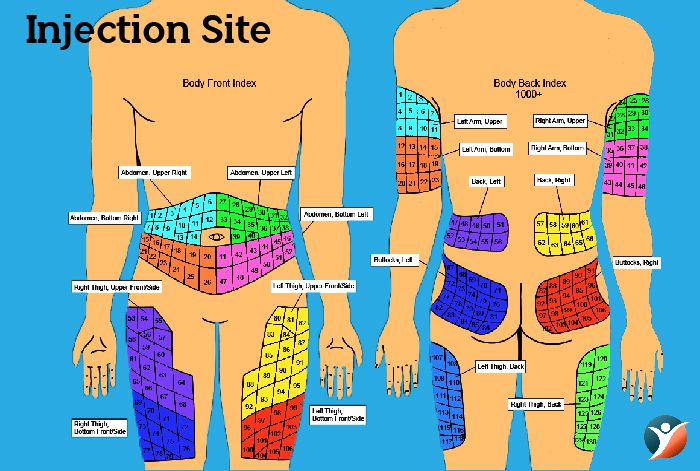
Injection should be given in the subcutaneous tissue of the upper arm and the anterior and lateral aspects of the thigh, abdomen and buttocks. Intramuscular injection is not recommended for routine delivery of insulin. It is important to rotate the injection site in order to prevent lipohypertrophy or lipoatrophy. It is recommended to rotate within one area rather than moving to a different area with each injection. This practice reduces the variation of absorption on a day to day basis.
Do’s and Don’ts of using Insulin Pens
Before using an insulin, following points should be checked:
- Expiry date
- Type of insulin
- Insulin is clear and transparent and not cloudy
Steps to administer insulin:
- Pen should be rolled gently between the palms and then gently tilted if an insulin mix is being administered.
- Pen cap must be removed and the top must be cleaned with the help of cotton wool.
- Needle should be attached to the pen. A new needle should be used every time.
- The pen must be primed and the required dose gets dialed up. Dose should be double checked before injecting.
- The site where the shot has to be administered must be cleaned. The cap removed and the pen held at an angle of 90 degree, unless instructed otherwise.
- The button should be pushed to deliver the dose. It is advised to wait for 10 seconds in order to make sure that all the insulin has been absorbed.
- The needle should be removed and disposed off properly.
Do’s and don’ts of Insulin Jet Injectors

Steps to Use Insulin Jet Injectors
- The pen must be loaded by filling the insulin adapter with insulin.
- The gauge must be set to the desired insulin dose.
- The device must be placed near the skin that has some fatty tissue like stomach, thighs and upper and outer section of buttocks.
- The button should be pressed to force a high-pressured stream of insulin through the small opening of the jet.
- The insulin converts into vapor and is absorbed through the skin and reaches the blood stream.
Calculating Insulin Dose

Commercially, insulin is available in the strength of 100 or 500 units/mL which is designated as U-100 and U-500 respectively. 1 unit is equal to nearly 36 micro grams of insulin. U-500 is prescribed to patients who have extreme insulin resistance.
The insulin dose is calculated as per the need and the disease of the person. It is extremely important to take a well calculated amount of insulin to avoid the risk of developing hypoglycemia.
Nearly 40-50% of the total requirement of insulin dose is used for replacing insulin overnight when the patient is fasting and in between the meals. This is called background or basal insulin dose that generally remains constant every day.
There remaining 50-60% of the dose is for carbohydrate coverage and is called bolus insulin replacement. This dose varies as per the carbohydrate content of the food consumed. The insulin to carbohydrate ratio is calculated to determine how many grams of carbohydrate are managed by 1 unit of insulin.
What happens when you do not take insulin?
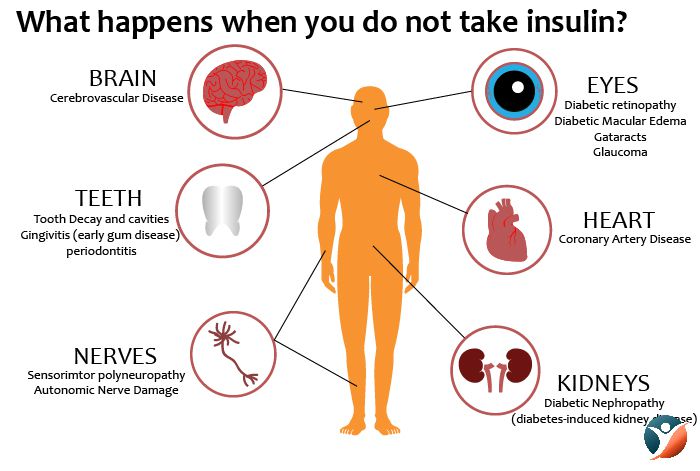
If a person has insulin dependent diabetes and he does not take insulin on a regular basis, it will cause glucose to build up in the bloodstream as the body is unable to move glucose from blood into cells. This excess glucose then gets excreted through urine which drags extra water to the urine, causing thirst and excess urination.
There is also a chance of developing dehydration due to water loss, that can result in confusion. In the absence of glucose in the cells, the cells can’t produce energy and therefore the person feels tired and loses weight.
If this continues for a long time, it can make the patient extremely ill. Gradually, the kidneys and retina of the eyes get damaged. If left untreated, the patient gets into coma and eventually die. If a person has been diagnosed with insulin-dependent diabetes, it is extremely important to take insulin.
How long Do you have to wait to eat before taking insulin?
The best time to eat after taking an insulin shot depends on the 3 major factors:
- Type of insulin being taken
- Type of food being consumed
- Current blood glucose levels
There are 2 major types of insulin that are taken before meals, namely rapid acting and short acting. It is advised to inject these insulin 15 minutes before meals. For short acting insulin, it is recommended to take it 30-45 minutes before meals. It should be noted that if a patient waits longer, there is a chance of developing severe hypoglycemia.
The type of food also determines the timing of insulin shot. Carbohydrate rich diet has a greater impact on the blood glucose level than protein rich diet. Fatty diets decrease the rate of absorption of carbohydrates from the gut.
The current blood glucose level also determines the time of insulin dose. If the blood glucose level is low and a dose of insulin is taken while still waiting for the food can cause a severe decrease in blood glucose levels that can be life threatening. However, if the glucose level is high and even then food is consumed, then a little extra dose of insulin might be required.
The amount of food that can be consumed by the patient depends on his weight, daily requirement of energy and the insulin to carbohydrate ratio.
It is extremely important to discuss these factors with a doctor who can guide the patient about how and when to take an injection of insulin.
What is Insulin Sliding Scale?
Sliding scale insulin therapy (SSI) is the dose of insulin that depends on the blood glucose level just before the meal. The higher the blood glucose levels, the more is the dose of insulin required. It is often used in a hospital setting where it is more convenient to monitor current blood glucose levels.
What Food Cause Insulin Resistance?

There are some foods that are responsible for spiking blood glucose levels, such as pastas, rice, soda and white breads. These foods are highly processed, digest very quickly and cause an increase in blood glucose levels very rapidly. This puts an extra stress on the pancreas, which is responsible for producing insulin. Some of the foods that should be included in the regular diet so that the body does not develop insulin resistance are as follows:
-
- Vegetables
- Beans and Legumes
- Fish
- Poultry
- Lean protein foods
- Whole grains
- Dairy
- Fruits
Why Insulin Should be Taken only on Prescription?
Self-medication with insulin should not be practiced under any circumstances because it can have serious repercussions like coma and even death from hypoglycemia. It is extremely important to take insulin under medical supervision. Insulin dose of each patient is tailored as per the needs of the patient and the type of disease.
Conclusion
Insulin is a boon for diabetic patients and latest advancements in the field of medicine have made this drug available to masses to better manage their disease. Various devices for administering this drug have been developed which are very user-friendly making life less painful for patients who need insulin therapy to keep their glucose levels in check. One thing that is very important to remember about insulin this boon can kill a patient if it is not properly used. So, it is very important to use it under the supervision of a doctor only.