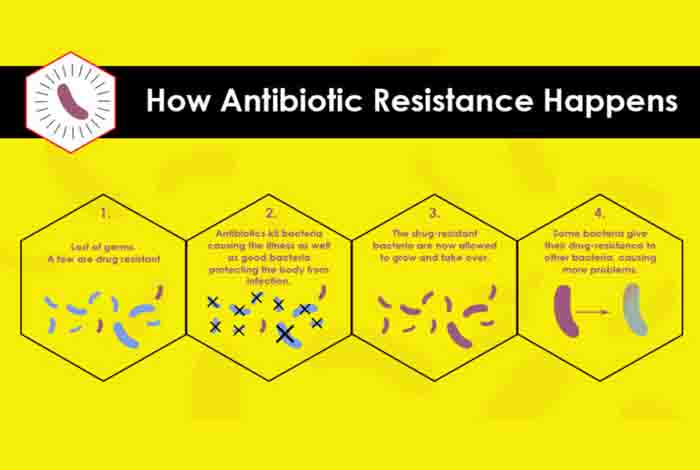
Bacteria can cause serious infections,. They can spread and even develop resistance to antibiotics. And, if these are not enough to scare you, then you must know the dire fact that they can also share their resistant weapons with other superbugs, allowing them to develop into a more resistant, unusual form, which is hard to be detected.
Dr. Anne Schuchat, Principal Deputy Director of Centers for Disease Control and Prevention (CDC), recently reported that they have found strains of highly antibiotic resistant bacteria that are the major cause of a series of infections. She further adds that these infections are very difficult or nearly impossible to treat, but through aggressive tests and examinations, they can put a halt on their worldwide spread.
According to CDC reports, nearly 2 million people get affected by antibiotic-resistant bacteria in the U.S., out of which, around 23,000 people die every year.[1]
You Might Be Affected with No Detectable Symptoms
CDC stated that they were taken by a surprise when they found 221 rare antibiotic resistant genes in 2017. When 11 percent of those examined for these superbugs, the results turned out to be positive with no apparent symptoms. The spread of these ‘nightmare bacteria’ is not only constrained to one city or state, but 27 states reported of their existence. Hence, it is important to stop them spreading before they engulf the whole world.
As a matter of fact, The WHO has also labeled the antibiotic resistant bacteria as a ‘threat to the entire human race.’[2]
How to Detect Them?
CDC has devised a new method to detect them as quickly as possible. They have put 500 of their staff members on a roll across the country to run certain tests and collect samples. This will help detect all those people, who have already been affected by such rare antibiotic resistant bacteria, and isolate them as soon as possible to restrict any more spread of these superbugs.
Dr. Lance Price, director of the Antibiotic Resistance Action Center at the George Washington University, said that inappropriate use and overuse of antibiotics by the people around is the major reason behind the development of antibiotic resistance in bacteria; both for the previous cases as well as the one in discussion.
He also said that for the nightmare bacteria, we as a human being are playing the role of an infected mosquito, helping the bacteria to spread further.
Opportunistic Superbugs
A healthy individual might become a carrier of such antibiotic resistant bacteria without being aware of it and may unknowingly transfer these bacteria to a susceptible person like a cancer patient, a weak elderly, fragile newborn baby or an immunocompromised person.
Since these people already have a weakened immunity to effectively fight off the nightmare bacterial infection, this gives the latter an opportunity to develop symptoms or worsen their conditions that may be even fatal.
According to Dr. Price speaks, the most important thing that CDC is currently emphasizing on is to detect the affected people and screen their relatives and social contacts too. This would certainly help eliminate nearly all possible chances of further spread of the nightmare bacteria.
Aggressive Approach to Check their Growth and Spread
CDC tested for the most highly resistant bacteria – carbapenem-resistant Pseudomonas aeruginosa (CRPA) and carbapenem-resistant Enterobacteriaceae (CRE).
Dr. Schuchat claims that only an aggressive approach can work against such highly antibiotic resistant bacteria. To confirm this, they compared the newly designed strategy with a more restrictive approach to fight off another kind of bacteria with resistance to antibiotic, known as extended-spectrum beta-lactamases (ESBLs). The results turned out to be more effective.
Incidentally, tackling these highly resistant bacteria with an intensive approach is not cost effective and a time-taking process. It may require a specialized laboratory to carry out the rapid detection, followed by infection control in all the hospitals, nursing homes that are affected along with finding the individuals, who are just carriers and may spread the infection.
Dr. Price emphasized that to overcome these barriers, there is a need of coordination between CDC, health care professionals, laboratories and health departments. Government funding is also important to combat challenges that these uncontrolled superbugs would pose in near future.
Dr. Price also suggests doctors getting a culture done before prescribing antibiotics in case a sick person approaches them. She further stressed on the need of point-of-care tests as this will ensure that the patients would get appropriately detected for the infection when they are still with their doctor.