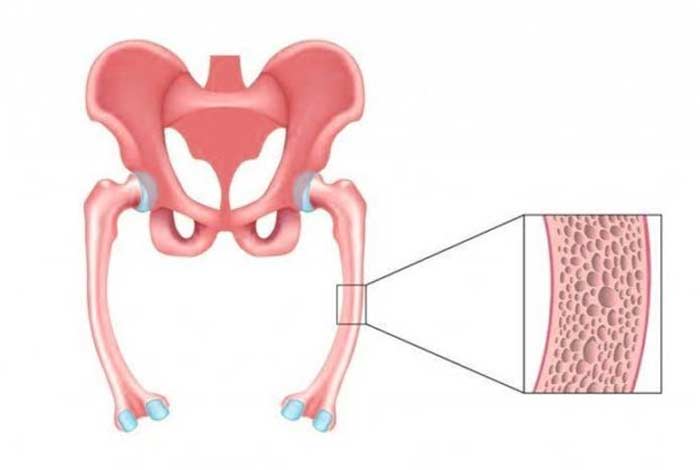
Bones are living tissues in the body that have their own blood vessels and are made up of living cells that grow and repair themselves. Bones are composed of two types of tissues, a hard, outer layer known as the cortical bone that is dense, strong and tough, and a spongy inner layer known as the trabecular or cancellous bone that is lighter and less dense than compact bone. It is a rigid organ that forms a part of our skeletal system. Bones provide the structure and support to the body and enable movement. The mineralized matrix of bone tissue is mainly composed of organic component, collagen and the inorganic portion is composed of different salts, like calcium phosphate.
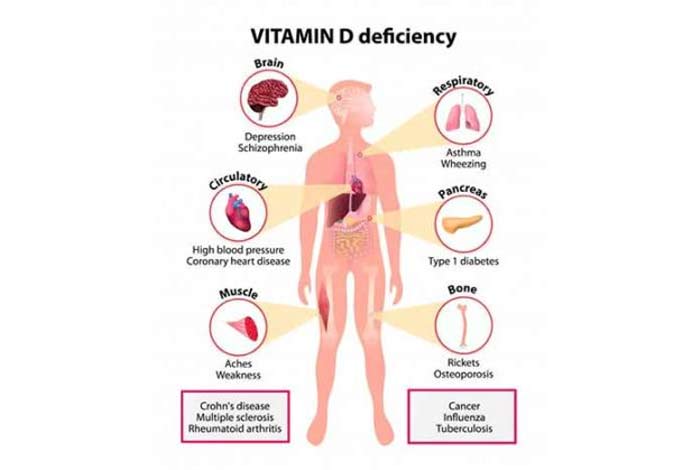
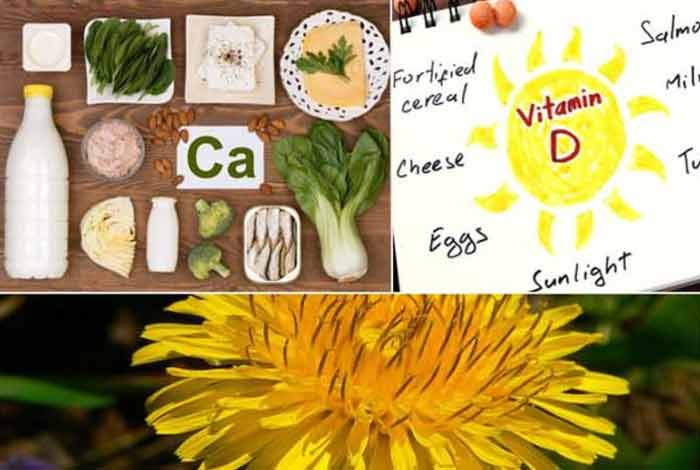
When we ingest foods rich in calcium and phosphorus, it is absorbed in the small intestine under the influence of parathyroid and thyroid hormones. [1] Vitamin D is also required in order to maintain a healthy balance of phosphorus and calcium in the blood. It is essential to keep bones in the prime of their health.
Vitamin D is very important in our body and deficiency of vitamin D can lead to diminished levels of calcium and phosphorus in our body. This can lead to a condition known as osteomalacia where the bones of the body become soft. Other conditions that can lead to softer bones are inadequate levels of calcium, and phosphate in the blood, and increased resorption of calcium from the bones due to impaired bone metabolism.
Osteomalacia can also develop due to secondary hyperparathyroidism, in which there is excessive secretion of a hormone from the parathyroid glands situated in the neck. Parathyroid gland is involved in regulating the calcium levels in the body. When the calcium levels become low in the blood stream, parathyroid gland secretes parathyroid hormone which increases the resorption of calcium from the bones into the blood stream. This process makes the bones soft and leads to osteomalacia. This situation corrects itself when vitamin supplements are given to the patient.
In children and young adults with osteomalacia, bones become soft and bowed, especially the weight bearing bones of the legs. Fractures are commonly seen in adults with osteomalacia.
Osteomalacia is different from the more common condition of mild vitamin D deficiency in the body, which is utterly common in the general population. For osteomalacia to develop, there needs to be severe deficiency of this vitamin. Also, osteomalacia and osteoporosis differ from each other as in the latter, there is thinning of bone due to decrease in bone density, thereby, increasing the susceptibility to fracture. In osteoporosis, the bones are porous and brittle, whereas in osteomalacia, they are soft.
Rickets is a disease that is seen in children, causing soft and fragile bones. It is commonly seen in children with severe deficiency of vitamin D in the body due to insufficient intake from the diet or when the body is unable to absorb and metabolize vitamin D properly. It can also be seen in children with calcium and phosphorus deficiency. This disease is known to produce more obvious skeletal deformities in children. When severe vitamin D deficiency leads to osteomalacia in adults, it becomes difficult to diagnose and to differentiate it from osteoporosis.
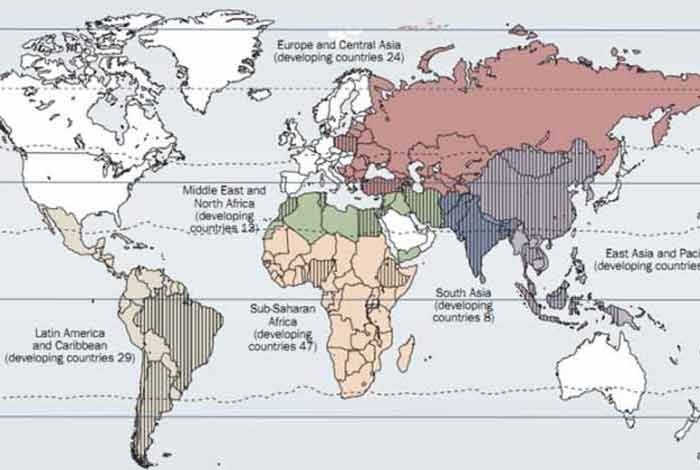
The number of cases of nutritional rickets and osteomalacia are escalating globally. Even the high -income groups are not left untouched by this disease.[2]
As surprising as it might seem, osteomalacia is not a rare condition and people all over world are its victims. As a matter of fact, in the U.S. alone, 1 out of every 1000 people is affected by this condition. Nearly 20-25 million Americans suffer from this condition, out of which approximately 25% are post-menopausal women. In kids, severe deficiency of vitamin D manifests itself as rickets and can result from environmental, dietary and genetic factors. It has been seen that the most common reason for vitamin D deficiency is its absence from dietary sources.
Symptoms of Osteomalacia
The onset of osteomalacia often goes unnoticed because the awareness about calcium deficiency is quite low among people. Since the symptoms are quite mild in the early stages, it is very difficult to identify it in its budding stage. As the sunlight becomes scarce in the autumn and winter months, vitamin D deficiency develops during these months.
However, osteomalacia resulting from vitamin D deficiency can display the following symptoms:
- Pain in bones
- Muscle weakness
- Slight cracks or partial fractures in the bone
1. Pain in Bones
Pain is most commonly experienced in the bones of legs, upper thigh, groin and knees and sometimes feet when the person is walking, standing or running. This pain can be eased by lying down or by sitting. Sometimes, even a minor knock on the bone can cause unusually high pain. With time, the person can feel pain throughout his body and even simple movements start hurting.
2. Muscle Weakness
Even the muscles are not spared from agony in this condition. They might start to feel weak or stiff. The most commonly affected muscles include those of thighs, shoulder and the main trunk. This can make it difficult for the patient to do simple tasks like getting up from chair without using the arm rest for support, climbing stairs and even getting out of the bed.
In some of the rarer forms of osteomalacia which are hereditary in nature, muscle weakness is not observed.
3. Bone Fractures
Fractures occurring in the body due to osteomalacia are partial in nature and are called Looser’s Zone. They can be highly painful. Occasionally, these partial fractures can even result in complete bone breaks.

Some of the other observed symptoms are:
- Feeling tired
- Painful spasms or cramps in the face, feet, hands due to low levels of calcium in the blood (rare)
- In rickets: bowed limbs (especially the legs), waddling gait, pot belly and disturbed growth
- Abnormal heart rhythm
- Numbness in arms and legs
- Numbness around the mouth
- Pigeon chest (forward protrusion of the chest bone)
- Impaired growth causing short stature
- Dental deformities
- Delayed tooth formation
- Insomnia
- Poor muscle development and tone
- Delayed walking in children
Risk Factors of Osteomalacia
Some of the factors that increase the risk of osteomalacia are as follows:
- Inadequate dietary intake of vitamin D, for instance due to lactose intolerance
Inadequate exposure to sunlight (ultraviolet radiation), which produces vitamin D in the body (increased risk in elderly people who are housebound) - Malabsorption of vitamin D by the intestines
- Inherited or acquired disorders of vitamin D metabolism
- Advanced kidney disease
- Phosphate depletion associated with low dietary intake of phosphates
- Certain medications such as those used to treat epilepsy
Do I Have Osteomalacia?
Osteomalacia is a condition which is extremely difficult to diagnose in its early stages. Majority of the people across the globe have vitamin D deficiency. However, when this deficiency becomes severe, only then osteomalacia develops. If you observe that your bones are getting fractured easily or there is development of partial fractures or Looser’s zone in the bone, there is a possibility that you might have osteomalacia. If your muscles feel weak or you experience bone pain, you should visit a doctor and get yourself properly checked. These are the symptoms of osteomalacia, which should not be dismissed lightly. The doctor can assess these symptoms and diagnose whether you have osteomalacia or any other bone disease such as Paget’s disease or osteoporosis.
Causes and Prevention of Osteomalacia
Osteomalacia is a condition that results due to defect in the maturation process of bones. The body requires calcium and phosphorus to build strong bones. If a person does not get these minerals in enough quantity through diet or the body is unable to absorb it properly from gut, it can lead to development of osteomalacia in that person. Given below are some conditions that can lead to osteomalacia:
1. Vitamin D deficiency
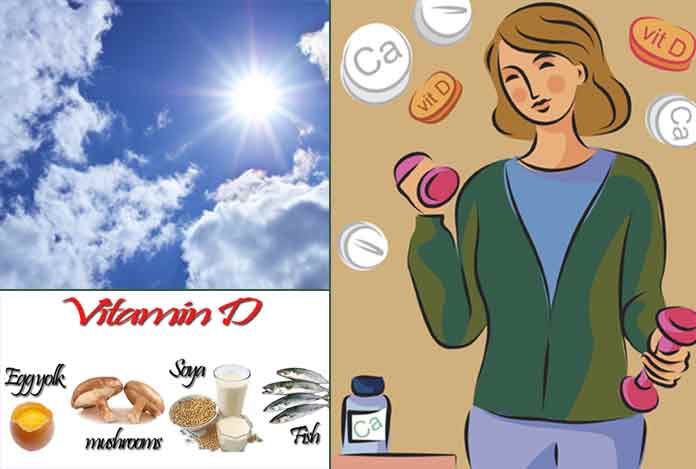
The skin is able to synthesize vitamin D in the body in the presence of sun. Also, it can be supplemented through the diet taken. However, people who live in areas where sunlight is scarce or do not get any exposure of sunlight on accounts of their occupation or by choice or consume foods that do not contain vitamin D are at a high risk of developing osteomalacia. Vitamin D deficiency can also occur in people whose bodies cannot absorb the vitamin properly from the gut. Globally, vitamin D deficiency is the leading cause of osteomalacia.
The daily requirement of vitamin D to protect the body from falling prey to osteomalacia is nearly 10 microgram/ day. The skin is capable of producing nearly 100 microgram/day of vitamin D which can be stored in the body for some time. A diet that provides about 10-20 microgram/day of vitamin D is enough to save you from osteomalacia. If the person does not get enough sun exposure, they need to supplement their diet with plenty of oily fish or vitamin D capsules.
2. Certain Surgeries
In the normal process, the food we eat gets broken down in the stomach to release vitamin D and other minerals which are then absorbed in the stomach. However, if the person undergoes certain surgeries to remove whole or a part of stomach, this process might get disrupted, causing vitamin D deficiency. Also, if a surgery is done to bypass or remove the small intestine, it can also lead to deficiency of vitamin D and calcium.
3. Celiac Disease
It is an autoimmune disorder in which consumption of food items containing gluten, a protein found in barley, rye and wheat, can cause potential damage to the inner intestinal lining of the small intestine. Due to this damage, the intestine is unable to properly absorb nutrients from the food and can be a stepping stone for vitamin D and calcium deficiency.
4. Kidney or Liver Disorders
Vitamin D requires to be activated in the body before it can show its effect. This activity is performed in the kidneys or the liver. If there is any serious disease of liver or kidney, this activation process can come to a halt, thereby decreasing the levels of active vitamin D in the body.
5. Drugs
Phenobarbital and phenytoin are the drugs that are used in the treatment of epilepsy. These drugs are known to cause severe vitamin D deficiency.
6. Hypo-phosphatemia
In hypo-phosphatemia, phosphate levels in the blood become abnormally low in the blood, which is generally seen in people who are malnourished, especially those who are suffering from chronic alcoholism. This causes the body to release hormones that causes resorption of phosphate from bones, paving way for softer bones. This condition results in muscle dysfunction and weakness as well.
7. Tumor Induced Osteomalacia
Oncogenic osteomalacia or tumor induced osteomalacia is a rare condition in which there is increased excretion of phosphate with urine. Such a situation arises when there is a benign tumor of soft tissue or bone present in the body. The tumor is generally small and is difficult to locate. As there is increased excretion of phosphate from the body, phosphate resorption from the bones takes place, that leads to softer bones.
8. Itai-Itai Disease
It is a type of cadmium poisoning that started in Japan and is characterized by extreme pain in spine and joints. Cadmium poisoning is also known to damage kidney and soften the bones. The bones become brittle and weak due to cadmium.

Prevention of Osteomalacia
Osteomalacia caused by inadequate sun exposure or a diet low in vitamin D often can be prevented by getting enough vitamin D. Foods that are rich in vitamin D and calcium should be consumed in larger proportions, like oily fishes, egg yolks. Even those foods that are fortified with vitamin can be consumed more often, such as bread, cereal, milk and yogurt. If need arises, vitamin D and calcium supplements can also be taken, after consulting a doctor. Unprotected sun exposure should be avoided as it can increase the chances of skin cancer. Experts still do not have a unanimous say on the duration of sun exposure required for preventing osteomalacia.
Diagnosis and Tests for Osteomalacia
Osteomalacia is a silent disease. It is difficult to diagnose it in the early stages. However, following are some of the tests that can be done to correctly diagnose osteomalacia:
1. Blood Test
Blood tests are performed to check the levels of vitamin D, calcium and phosphorus in order to determine if the person has any kind of bone abnormality. Tests are also performed to determine the levels of alkaline phosphate isoenzyme and parathyroid hormone levels. Abnormal levels of these hormones indicate osteomalacia.
2. Imaging Scans
The small partial fractures, called Looser’s Zones, that is commonly found in people with osteomalacia can be observed with the help of X ray and other scans. Even a small injury can result in major fractures in these people. Therefore, if osteomalacia is suspected, scans should be performed.
3. Bone Biopsy
Biopsy involves removing a tissue from the body to diagnose a disease. In order to correctly diagnose osteomalacia, bone biopsy is done in which a small tissue is removed from the bone and tested. A tiny needle is inserted and a sample of bone is taken which is examined under the microscope for signs of osteomalacia. Usually, an X-ray and blood tests are enough to make a diagnosis and a bone biopsy isn’t necessary.
4. Bone Density Test
In people with osteomalacia, the bone density decreases, which can be diagnosed with Dual Energy X-ray Absorptiometry or (DEXA). Through this test, the density of calcium and other minerals of the bone is tested. Even if the results come back negative for osteomalacia, predictions can be made if the person is at a high risk of developing the disease. Weaker bones are indicated by the lower mineral content.
Treatment and Care of Osteomalacia
If an early diagnosis of osteomalacia is made, the treatment is simple. Taking supplements of vitamin D, calcium and phosphate can help in curing the disease. If vitamin D deficiency occurs after an intestinal surgery or injury, or if the person consumes a diet low in vitamin D, supplements is the first line of treatment. In rare cases, vitamin D injections can be given through the skin or intravenously. Doctors might also recommend spending some time in the sun to facilitate vitamin D synthesis by the skin. If any other health condition such as liver cirrhosis or kidney disease is causing deficiency of vitamin D, they should be treated accordingly. In severe cases of osteomalacia or rickets, children might be suggested to wear braces or undergo surgery to correct their bone deformation.

Care of Osteomalacia
Osteomalacia is a condition which has high possibility of recurrence. There are high chances for the disease to return with similar symptoms like broken bones in legs, spine and ribs, which require immediate medical intervention. Including Vitamin D-rich food in your diet like yogurt bread, egg yolks, milk, cereal and oily fishes can come in handy in preventing the disease.
If due to any reason, these food items cannot be included in the diet or the person has difficulty in absorbing nutrients from the gut, vitamin D supplements can be easily taken. Also, sun exposure can also help in bringing your vitamin D levels back to normal and substantially reduce your chances of developing osteomalacia. However, as the saying goes, excess of everything is bad, too much exposure to sun can have adverse effects on your skin and therefore, before going to the sun for your dose of vitamin D, consult a dermatologist.
Exercise also acts as a boon for the osteomalacia patients as it can help in getting rid of muscle stiffness and weakness, which develops in the later stages of disease. Weight-bearing exercises like walking can play an important role in strengthening bones and muscles. However, high intensity exercises should be avoided until Looser’s fractures get healed.
If persistent symptoms of numbness, difficulty in moving joints or swelling is observed, seek medical consultation as soon as possible. However, if serious symptoms like severe swelling, inability to sense the bone or dislocation is observed, it is advised to get medical help immediately.

OTC medications and Self Management Methods Available
Vitamin D and calcium supplement tablets are generally available over the counter in most of the pharmacies. These supplements can be taken under the supervision of a doctor for preventing the bones from becoming soft.
Self Management of Osteomalacia
Eating food items that are rich in vitamin D, regular exercise and adequate exposure to sunlight can go a long way in managing osteoporosis. Occupational therapies can also help the patients in making their lives easy by teaching the coping strategies and providing aids and equipments. As osteoporosis progresses, the chances of falling also increases which should be discussed with a physiotherapist, occupational therapist and the doctor.

Natural Ways to Cure Osteomalacia
1. Get Enough sunshine
For more than 500 years, vitamin D, has been produced on this planet. [3] Skin is the organ that is responsible for synthesizing vitamin D. When the sunlight penetrates the skin it converts provitamin D3 to previtamin D3 [4]. However, season, time of day, altitude, skin pigmentation, latitude, sunscreen use and aging affects the synthesis of sun induced vitamin D. If a person is exposed to sun for a suitable amount of time each day, its vitamin D deficiency can be countered. It should be noted that vitamin D cannot cure osteomalacia on its own. It simply promotes better absorption of calcium and phosphorus from the gut that can make the bones stronger.
A study done by the Naval Submarine Medical Research Laboratory, U.S.A. in 2005 showed that 6 days of sun exposure is enough to counterbalance 49 days of sun-less days. However, some experts question the number of days of sun exposure that are required to prevent soft bones.
The person can be exposed to mild sun in the morning hours for 15-20 minutes, but if the skin is richer in melanin, sun exposure can be increased. While getting sun exposure, tight clothes should be avoided. While going out at noon, use of sunscreen is suggested to avoid skin damage and cancer.
2. Cod Liver Oil
The yesteryears doctors have trusted cod liver oil for protecting bones against osteomalacia and other diseases like rheumatism, stiff muscles and aching joints. Cod liver oil is rich in vitamins D, A and omega 3 fatty acids, that can help in making bones and muscles strong and protects against type I diabetes and hypertension.
3. Oily Fish
Fish is a super food that is known to possess a number of health benefits. It has natural vitamin D that can help in preventing bones from becoming soft. Some of the fish varieties that are rich in vitamin D are:
- Sardines
- Mackerel
- Pilchards
- Fresh tuna
- Salmon
- Catfish
4. Calcium Rich Diet
While consuming foods rich in vitamin D is essential for protecting bones from becoming soft, calcium rich diet is equally important. When the levels of calcium and phosphorus are low in the blood, the body starts producing hormones from the parathyroid and thyroid gland for calcium resorption from bones, increasing the vulnerability of bones to turn soft. Therefore, it is absolutely necessary to consume a diet rich in calcium as well. Some of the food items that can be included in the daily food platter for giving the body a boost of calcium are:
- Dairy products like milk, yogurt and cheese
- Soybeans and tofu
- Leafy green vegetables like broccoli and cabbage
- Nuts
- Fish whose bones are also eaten like sardines and pilchards
the bones While lack of vitamin D leads to non-absorption of calcium by the body, there is yet another consequence of not having dietary calcium. When the minerals, calcium and phosphates, lower in the blood, the body starts producing hormones which cause calcium and phosphate to be released from the bones. This results in weak and soft bones. Therefore, along with vitamin D, calcium rich diet is also essential to prevent and cure rickets.
5. Dandelion
Dandelion herb is rich in vitamins like vitamins A, B complex, C and D, and minerals like magnesium, zinc, potassium, iron, manganese, calcium, copper, boron, silicon and iron. It is one of the most commonly recommended herbs for the managing osteomalacia through natural ways.
Health Tip By Experts
Osteoporosis might seem as a debilitating disease, but can be easily managed through lifestyle and dietary changes. Vitamin D is the key to healthy and strong bones and foods rich in vitamin D should be included in the daily platter. Also, a little friendship with the sun will go a long way in preventing osteomalacia.