
Inflammatory Bowel Disease – Types, Symptoms, Risk Factors and Treatment

Overview and Facts
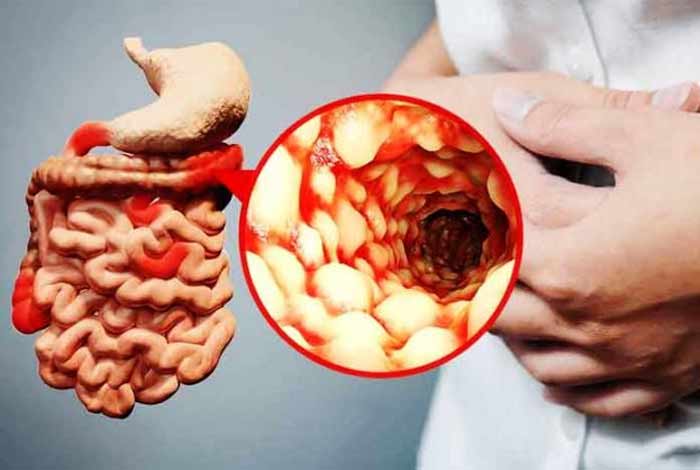
Inflammatory Bowel Disease (IBD) constitutes a group of disorders in which there is an inflammation of the digestive tract. Inflammation is a condition in which there is a local response to a triggering factor which is marked by dilation of blood vessels, redness, heat, and pain. The triggering factor can be an infection, irritation or injury. IBD is often considered as an autoimmune disorder but it might also be due to the attack of the immune system on a virus, bacteria or food in the digestive tract leading to inflammation and subsequent bowel injury.
There are two types of IBD, namely; Crohn’s Disease (CD) and Ulcerative Colitis (UC). These two differ in the type of inflammation produced by them. In Ulcerative Colitis inflammation is limited to the large intestine only whereas in Crohn’s Disease, there is inflammation throughout the length of the digestive tract and it is severe in the small intestine.
Ulcerative colitis is the most prevalent form of IBD in the world. Its occurrence varies according to geography, with most cases being reported in western countries. In 2015, approximately 1.3% of Americans were diagnosed with IBD which showed an increase from a mere 0.9% in 1999.
CD is about four times more common in adults than in children. People are generally diagnosed with CD in their adolescence or early adulthood, between the age of 15-35 years. IBD is more common in whites than African Americans, Asians, and American Indians. Studies have shown that the disease is becoming increasingly common in children and adults. Males are at a slightly higher risk of developing CD than females.
Types and Symptoms of Inflammatory Bowel Disease
Types of Inflammatory Bowel Disease:
There are three types of IBD, namely:
- Crohn’s Disease
- Ulcerative colitis
- Intermediate Colitis
1) Crohn’s Disease
It is an inflammatory disease affecting any part of the digestive tract, most common being the end of the small intestine, known as ileum, or the colon. In this disease, the inflamed areas are patchy, with small sections of normal intestinal wall in between. The inflamed portion can be small or large. It might also penetrate into the deeper layers of the digestive tract.
The disease can cause very painful symptoms and be debilitating and might even be life-threatening. With therapy, it’s signs and symptoms can be reduced, and the disease can be managed well with proper treatment.
Some symptoms of Crohn’s disease are:
- Diarrhea
- Abdominal cramps and pain
- Constipation
- Tiredness and fatigue
- Feeling unwell
- Loss of appetite
- Unintended weight loss
- Increased body temperature
- Joint pain and swelling
- Inflammation and irritation of eyes
- Patches of painful, red and swollen skin, generally on legs
- Mouth ulcers
- Slow growth rate in children
Types of Crohn’s disease:
a) Ileocolitis
In this type of CD, the ileum and the colon get inflamed, generally on the right side. About half of the people diagnosed with Crohn’s disease have ileocolitis. This is a lifelong condition which cannot be treated completely. In severe cases, fistulas (furrows), strictures (thickened colon wall), colon cancer, abscesses (pockets of pus) can be formed, along with malnutrition.
Symptoms are:
- Diarrhea
- Fatigue
- Weight loss
- Cramping in the right lower side or middle of the abdomen
b) Ileitis
in this, there occurs inflammation in the ileum. This affects about 30% of the people suffering from Crohn’s disease. Complications that can arise out of ileitis include fistulas, strictures, abscesses, and malnutrition.
Symptoms are:
- Diarrhea
- Weight loss
- Fatigue
- Cramping in right lower part or middle of the abdomen
c) Gastroduodenal Crohn’s Disease
In this type, there is inflammation of the esophagus (food pipe), stomach and/or duodenum (first part of small intestine). Only about 5% of the people diagnosed with Crohn’s disease develop gastroduodenal Crohn’s. In a complicated case, fistulas, gastroduodenal strictures, gastric outlet obstruction, pancreatitis, and abscesses can develop along with nutritional deficiencies.
Symptoms are:
- Loss of appetite
- Weight loss Nausea
- Vomiting
- Abdominal pain similar to indigestion
- Fatigue
d) Jejunoileitis
In Jejunoileitis there occurs inflammation in the jejunum, the upper half of the small intestine. It is more common among children than adults. It is an uncommon type of Crohn’s disease. Complications include the development of fistulas, strictures and nutritional deficiencies.
Symptoms are:
- Cramps after meal
- Diarrhea
- Intense abdominal pain
- Weight loss
- Anemia
- Fatigue
e) Crohn’s (Granulomatous) Colitis
Here the inflammation occurs only in the colon or the large intestine and affects about 20% of the people suffering from CD. There is a misconception that Crohn’s Colitis implicates having Crohn’s disease along with ulcerative colitis. Colitis simply indicates inflammation of the colon and has no connection with ulcerative colitis. Complicated cases might develop colon cancer, strictures, fistulas or abscesses.
Symptoms are:
- Blood stained diarrhea
- Rectal bleeding
- Lesions on skin
- Join pain
- Ulcers, fistulas, and abscesses near anus
- Fatigue
f) Perianal Crohn’s Disease
In this type of Crohn’s disease inflammation occurs around the anus which can occur alone or along with some other form of CD, leading to inflammation in other parts of the digestive system. It affects about a third of the people suffering from CD. In severe cases, fistulas, abscesses, rectal strictures, ulcers, skin tags around anus and fissures or tears in the lining of anal canal might occur.
Symptoms are:
- Pain and/or itching around the anus
- Bleeding with pus/mucus from anus
- Urgency to pass stools
2) Ulcerative Colitis
In Ulcerative colitis there is inflammation of the large intestine, also called colon. This inflammation is long lasting and produces ulcers in the digestive tract, affecting the innermost lining of colon and rectum. Symptoms develop gradually and are not evident immediately.
It can be crippling and can even lead to life-threatening complications. With treatment, the signs and symptoms can be managed effectively and might even bring about long-term remission.

Common symptoms are:
- Diarrhea
- Abdominal pain and cramping
- Rectal pain with rectal bleeding
- Urgency to defecate yet cannot
- Weight loss
- Fatigue
- Fever
- Slow growth rate in children
Types of Ulcerative Colitis:
a) Ulcerative Proctitis
In this type of UC inflammation is localized to rectal area and rectal bleeding might be the only sign of this disease. It affects only about 6 inches of the rectum or less. For about 30% of the patients, the disease develops starts in this form. It is considered as a less severe form of UC and causes fewer complications.
Symptoms are:
- Diarrhea
- Blood stained stools
- Rectal pain
- Urgency to defecate
b) Proctosigmoiditis
It affects the rectum and lower segment of the colon or the sigmoid colon which is the last section of the colon.
Symptoms are:
- Diarrhea
- Blood stained stools
- Cramps in abdomen
- Urgency
- Pain on the left side of the abdomen
c) Left-sided colitis
This is known as limited or distal colitis because there is inflammation in the left side of the colon i.e. in the rectum, sigmoid colon, and descending colon.
Symptoms are:
- Diarrhea
- Bloody diarrhea
- Weight loss
- Loss of appetite
- Occasional severe left-sided abdominal pain
d) Pancolitis
This condition arises when there is inflammation throughout the colon.
Symptoms are:
- Diarrhea, more than 6 stools a day
- Cramps in the abdomen
- Weight loss
- Severe abdominal pain
- An expanded colon as seen in an X-ray
- Fever, rapid heartbeat with anemia
e) Acute severe ulcerative colitis
In this rare form of UC, the entire colon is inflamed.
Symptoms are:
- Severe pain
- Profuse diarrhea
- Bleeding
- Fever
- Inability to eat
Difference between Ulcerative Colitis and Crohn’s Disease
| Ulcerative Colitis | Crohn’s Disease |
| Limited only to colon | Occur anywhere between moth and anus |
| Continuous inflammation of the colon | Patches of healthy tissue in between inflamed area |
| Only affects innermost lining of the colon | Occur in all the layers of the bowel walls |
3) Indeterminate Colitis
In some cases, it becomes difficult to determine whether the disease is Crohn’s Disease or Ulcerative Colitis. In such cases, the patients are diagnosed with indeterminate colitis. It occurs in about 10-15% of cases of IBD. Most of the patients are eventually diagnosed either with UC or CD later. This difficulty in diagnosis occurs because of the low sensitivity of the diagnostic tests.
Risk Factors for Inflammatory Bowel Disease
According to the Crohn’s & Colitis Foundation of America (CCFA), approximately 1.6 million people in the U.S. have IBD. The exact causes of developing IBD are rather unknown but there are some factors which increase the probability of developing IBD:
1) Geography
People living in western countries are at a higher risk of developing IBD. This could be due to lifestyle choices, more consumption of processed food or due to pollution. Developing countries are showing an increase in cases of IBD being reported every year may be due to easier access to processed food and increasing levels of pollution.
2) Age
UC and CD are more likely to be diagnosed during adolescence and early years of life. However, people can get this disease later in life too. Younger patients tend to have a more aggressive form of the disease as in them, the genetic factor plays a role in developing the disease. In older people, it is due to environmental factors.
3) Smoking
Smoking is one of the major factors responsible for developing Crohn’s disease. It aggravates the pain and other symptoms related to CD and also escalates the chances of developing complications. UC is found to be more common among non-smokers and ex-smokers.
4) Appendicitis
Young people who have undergone appendicitis are at a lower risk of developing UC due to alteration in the way the immune system works. The reason for this is not fully known. However, having the appendix removed after the development of disease has no effect on the course of the disease.
5) Genetics
Genetics plays a role in predisposing an individual to develop Jejunoileitis IBD. It has been found that if a twin develops CD, then there is a 50% chance that the other twin will develop the disease too during his lifetime. In case of UC, it comes down to 6%.
6) Parasites
It is theorized that since humans have less number of parasites living in their internal system, they are more likely to develop IBD, especially due to less prevalence of Helicobacter pylori infections in early childhood. It is found that in developed countries where H. Pylori infections are less prevalent, the incidences of IBD increased. It is postulated that H. pylori infections might protect against IBD by increasing the expression of genes that help in regulating the function of WBCs.
7) Medications
There are a few medications which increase the risk of developing IBD like contraceptive pills, hormone replacement pills for menopausal women, acne medication like Accutane and NSAIDs like ibuprofen.
8) Diet
Scientists have found that consuming a lot of animal protein increases the risk of developing CD. Diets rich in fat and sugar also contribute to increasing the risk of IBD.
9) Ethnicity
People of Northern European or Ashkenazi Jewish descent are at a higher risk of developing IBD. African Americans have a low risk of developing IBD but if they get it then they often require surgery to correct their condition.
10) Colon Bacteria
Common food poisoning causing bacteria such as campylobacter and salmonella have been linked with increased the risk for developing IBD.
Do I Have Inflammatory Bowel Disease?
If you have regular cramps in the abdomen along with bloody diarrhea, you may have IBD. Increased urgency to go to the bathroom to defecate along with the above-mentioned symptoms point to the fact there is something wrong with your system and you must not delay in consulting a doctor. Loss of appetite and considerable weight loss along with fatigue too can be symptoms of IBD.
You must visit a health care provider and get yourself thoroughly examined as bloody stools can also a be due to hemorrhoids or intestinal tear which might require an immediate medical attention. Abdominal pain is a rather common symptom can be due to a variety of reasons such as gas pains, indigestion or a pulled muscle which can be easily managed. Even when diagnosed with IBD, you must not panic as that might flare up the symptoms and cause more distress.

Causes and Prevention of Inflammatory Bowel Disease
Causes of Inflammatory Bowel Disease:
The exact cause of IBD is not known. However, there are indications which point to the involvement of immune system and genetic predisposition contributing to the development of IBD.
1) Genetic predisposition
It is generally observed that if there is a family history of IBD, the children are more susceptible to developing IBD. Certain gene mutations predispose a person to develop IBD.
2) The immune system
Any bacterial or viral infection of the digestive tract can provoke an immune response, leading to inflammation. When the infection is cured, the symptoms vanish too. However, in people suffering from IBD, such inflammation in the digestive tract can occur even in the absence of disease due to an abnormal response of immune system to bacteria, virus, food particle etc. IBD occurs when the inflammation is persistent for a long time.
3) Bacteria or viruses
Studies indicate that there is a relationship between E. coli and enteroviruses infection and CD.
4) Others
Smoking, oral contraceptives, diet, and antibiotics are known to be potential causes for IBD. High protein diet is known to be associated with IBD as it has a high content of sulfur which has a role in developing IBD.
Prevention of Inflammatory Bowel Disease:
Following methods can be used to prevent IBD:
1) Smoking cessation
Smoking is a cause for developing CD. It is also known to increase the chances of developing complications in CD patients. Hence, quitting smoking might help in lowering the risk of developing CD.
2) Physical activity and Exercise
Some studies have shown that having moderate physical activity helps in increasing the overall quality of life without having any detrimental effect on disease activity. Physical fitness might aid in reducing systemic inflammation levels. Low fitness levels are associated with increasing the risk of developing IBD.
3) Nutrition
A diet rich in saturated fats and low in fiber is associated with increasing the risk of developing IBD. However, no particular diet is defined which can improve disease course in adults with IBD. Increased consumption of cruciferous vegetables is associated with lowering the risk of the CD but not UC.
4) Environment
There are many studies which show that people who work outside, were breastfed during infancy and belong to the middle-lower socio-economic background are less prone to develop IBD.
5) Stress
Although not linked directly to cause IBD, stress might trigger an inflammatory response and aggravate the symptoms of this disease. Hence, it is advised to reduce stress.

Diagnosis and Tests for Inflammatory Bowel Disease
Following methods are used for diagnosing IBD:
1. Blood tests
- Tests for anemia or infections
- Fecal occult blood test
2. Endoscopic procedures
- Colonoscopy
- Flexible sigmoidoscopy
- Upper endoscopy
- Balloon-assisted enteroscopy
3. Imaging procedures
- X-ray
- CT scan
- MRI
1. Blood Tests:
- Tests for Anemia or Infection: Blood tests might be conducted to check for anemia or any infection which might suggest IBD.
- Fecal Occult Blood Test: Stool tests are conducted to determine the presence of hidden blood in person’s stools.
2. Endoscopic Procedures:
- Colonoscopy: In Colonoscopy, a thin, flexible, lighted tube is used to examine the rectum and sigmoid colon. During the procedure, small samples of intestinal tissue are taken for laboratory analysis to help confirm the diagnosis.
- Flexible Sigmoidoscopy: A slender, flexible, lighted tube is used in this method to examine the rectum and sigmoid portions of the colon. This method is used when the colon is severely inflamed.
- Upper Endoscopy: Here a slender, flexible and lighted tube is used to examine the esophagus, stomach, and duodenum. This is recommended in cases when the patient is having nausea, vomiting, difficulty eating or pain in upper abdomen.
- Capsule Endoscopy: In this, the patient is made to swallow a capsule which has a camera fitted inside it which captures the images of the intestine and sends it to a recorder fitted onto a belt worn by the patient. The capsule exits the body through the stool, painlessly. This is used for diagnosing CD.
- Balloon-Assisted Enteroscopy: In this, a scope is used along with an overture which enables the doctor the doctor to look further into the small intestine where normal endoscopes cannot reach. It is used when some irregularities are observed through capsule endoscopy.
3. Imaging Procedures:
- X-Ray: A standard X-ray technique might be used in cases of severe IBD to rule out any complications like a perforated colon.
- CT Scan: By using this test, the entire bowel can be scanned along with the surrounding tissues to help diagnose IBD.A specialized version of CT scan, known as CT enterography provides better images of the bowel.
- MRI: In this, a detailed image of organs and tissues is created by using a magnetic field and radio waves. It is used to evaluate fistula around the anus or small intestine and is known as pelvic MR and MR enterography, respectively.
4. Barium Enema: In this barium sulfate and the air is used to outline the lining of rectum and colon which can show polyps, tumors or diverticulosis.

Treatment and Care of Inflammatory Bowel Disease
The treatment for IBD has three main aims:
- To prevent symptoms
- Ease symptoms
- Improve the quality of life
These are the treatment methods used for treating and managing IBD, namely:
- Aminosalicylates
- Corticosteroids
- Immunomodulators
- Antibiotics
- Biologics
Other medications
- Anti-diarrheal medications
- Pain relievers
- Iron supplements
- Calcium and Vitamin D supplements
- Surgery
The current standard approach for treating IBD is the ‘Bottom-Up Approach’ which means assessing the symptoms and then choosing the treatment accordingly. This implies that if a patient has mild symptoms, he will be treated with aminosalicylates or antibiotics. People with more severe symptoms are given corticosteroids and in very severe cases, the patient is prescribed with biologics or surgery.
1) Aminosalicylates
Aminosalicylates are used for treating people with UC or mild forms of CD as they reduce inflammation in the digestive tract. They can be taken as syrup, tablet or as suppository depending on the location of the inflammation. Some of the commonly prescribed drugs are sulfasalazine, olsalazine, mesalamine etc.
2) Corticosteroids
Since IBD is an inflammatory disease, drugs like dexamethasone, hydrocortisone, methylprednisolone which reduce inflammation can be used. These are used when the symptoms flare up and require immediate treatment. But, these drugs are not prescribed for long-term therapy because of serious long-term side effects. These drugs can be taken as tablets, suppository or even as an injection.
3) Immunomodulators
Immunomodulators act by altering the activity of immune system. They suppress the overactive immune system and bring relief. They can be prescribed for long-term therapy because they take at least six months to start acting. They are prescribed along with corticosteroids until they begin to show effect. They are taken orally as tablets or are injected. Some of the drugs prescribed are 6-mercaptopurine, cyclosporine A, methotrexate, azathioprine, tacrolimus etc.
4) Antibiotics
Broad-spectrum antibiotics are used for treating bacterial infections resulting from abscesses or fistulas or those arising due to the infection of Clostridium difficile. These are generally prescribed after surgery to prevent any post-surgery infections and are given in the form of tablets or as injections. Some of the commonly prescribed antibiotics are metronidazole, ciprofloxacin, rifaximin etc.
5) Biologics
These are the proteins that stop certain molecules in the body from causing inflammation in the digestive tract. These are prescribed in patients who show a low response to other treatments methods. These are administered as injections or IV infusions. Some of the drugs prescribed are infliximab, adalimumab, certolizumab, natalizumab, and vedolizumab.
6) Other Medications and Supplements
In addition to the above-mentioned medications, some other types of medications are prescribed to aid in the management of this disease. These must be taken only under medical supervision.
- Anti-diarrheal Medications: For alleviating diarrhea, fiber supplements such as psyllium powder or methylcellulose are prescribed to help relieve mild to moderate diarrhea by adding more bulk to the stool. For more severe diarrhea, loperamide may be used.
- Pain Relievers: For managing mild pain, acetaminophen can be prescribed. However, NSAIDs such as ibuprofen, naproxen sodium, and diclofenac sodium are generally avoided as they pose the danger of causing gastrointestinal toxicity in the form of erosions, ulcers, colonic bleeding and rarely perforation and obstruction.
- Iron Supplements: If the patient has chronic intestinal bleeding, he might develop iron deficiency anemia and require iron supplements.
- Calcium and Vitamin D Supplements: CD and use of steroids increase the patient’s chances of developing osteoporosis. Hence, calcium and vitamin D supplements might be needed.
7) Surgery
If any of the above-mentioned treatments do not work out, surgery is recommended.
- Surgery for UC: Surgery can help in getting rid of the symptoms of UC, but it involves removing the whole colon and rectum. In most cases, it involves the construction of a pouch from the end portion of the small intestine for collecting stool. It is directly attached to the anus. This procedure is known as Ileal pouch-anal anastomosis. If construction of pouch is not possible, then a permanent opening is created in the abdomen through which stool is passed and is collected in a bag worn by the patient.
- Surgery for CD: Almost half of the people suffering from CD require surgery at some point. However, surgery does not cure the disease completely. During surgery, the damaged portions of the digestive tract are removed, and the healthy portions are joined together. Surgery might also be used to close fistulas and drain the abscesses that emerge due to complications. The disease is known to recur near the sewed healthy tissue. Medication and surgery should be followed simultaneously for managing the disease.

OTC Medications and Self-Management Methods for Inflammatory Bowel Disease
There are no over-the-counter drugs available for managing IBD as it is a chronic inflammatory condition. However, some drugs can be obtained for managing the symptoms such as loperamide for managing diarrhea or anti-gas products for bloating like simethicone. For managing pain, acetaminophen can be taken, but not other NSAIDs. All other medications should be taken only under medical supervision.
For self-managing the disease, following lifestyle changes can be done:
- Change in Diet and Meal Pattern: Irritating food should be avoided which can flare up the symptoms. Alcohol, caffeine, raw fruits, and vegetables etc. should be eliminated from the diet completely. Bland foods like fruit juices, banana, lean meats, fish, tofu etc. must be eaten. Frequent small meals should be encouraged instead of large meals. When the disease is in remission, balanced diet should be taken which contains food rich in soluble fiber, lean proteins, good fat and rich in calcium.
- Physical Activity: When the disease is in remission, plenty of physical activity should be undertaken to restore the quality of life. Physical activities should be planned around the patient’s bowel patterns when the stomach is mostly empty.
Natural Ways to Cure Inflammatory Bowel Disease
There are a few natural methods that can be used to manage the symptoms of IBD. Some of them are:
- Sitz baths can be taken by the patients in which the rectal area is soaked in lukewarm water for 15 minutes, two to three times a day for three weeks.
Compresses saturated with ice packs and pomegranate juice can be applied to the anal area. This provides instant relief to the inflammation. Ice should be wrapped in soft cotton cloth and should be kept only for a short time. - Mild exercise might help in treating CD as it relieves depression, heals bowel problems and reduces stress. It is also known to normalize bowel function. Regular relaxation and breathing exercises can assist in managing stress.
- Consumption of red clover helps in decreasing inflammation and helps in healing IBD.
- Increased intake of cod liver oil helps in managing IBD as it has high concentrations of omega-3 fatty acids.
- Intake of two cups of aloe vera juice half cups twice a day helps in managing IBD. However, it should be avoided during pregnancy or breastfeeding.
- Steamed apples help in healing fissures and ulcers and are very useful in managing IBD in its severe form.

Health Tip by Expert
IBD is a disease that can be debilitating in its nature but with proper medical care, it can be managed effectively. By following proper diet and exercise, the symptoms can be treated. Self-medication should be avoided, and proper treatment should be followed. With appropriate care and treatment, a fulfilling life is possible.





