Introduction
Diabetes is emerging as a global epidemic that is bound to have a devastating effect on the physical, financial and emotional health of people all over the world. Diabetes refers to a group of metabolic diseases which result in elevated levels of glucose in blood as well as urine of an affected person. When we eat food, various digestive enzymes act on it and break the complex carbohydrates into a simple sugar, glucose. This glucose is absorbed by the blood from the gut, which raises the blood glucose levels. Insulin senses the change in blood glucose levels and signals the liver, muscles and fat cells to take up this glucose to utilize it for energy production. If the body has enough energy, insulin signals the liver to store the excess glucose by converting it into glycogen through a process, glycogenesis.
When our body does not produce enough insulin or the cells of the body fail to respond to insulin and take up glucose from the blood stream, the blood glucose levels in the body starts to increase. This results in perpetually high levels of glucose in blood, leading to diabetes.
For decades, scientists and the medical community have identified two types of diabetes, Type I (T1DM) and Type II (T2DM). Type I diabetes is a condition in which the pancreatic cells synthesizing insulin are attacked by the body’s immune system and destroyed. Therefore, the pancreas fails to produce insulin and the glucose levels in the blood increase. In type II diabetes, the pancreas continues to produce insulin but the body stops responding to it. This leads to decreased uptake of glucose from the blood and the glucose levels remain high in the blood. Increased blood glucose level signals the body to produce more insulin. When this excessive production of insulin is continued for a long period of time, the insulin producing beta cells of pancreas wear out and can no longer produce insulin. This causes a perpetually raised blood glucose levels.
Till recently, any kind of perpetually raised blood glucose levels arising out of pancreatic dysfunction was classified into type II diabetes and was treated accordingly. But the recent findings suggest something different.
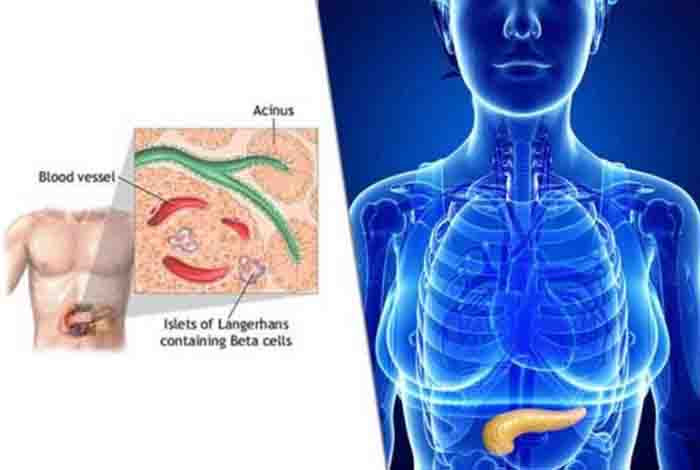
Physiology of Pancreas
Pancreas is a glandular organ located in the abdomen and is a part of the digestive system. It plays a major role in digesting the food and in regulating the blood glucose levels. Two primary functions are served by this wonderful gland, production of digestive enzymes for digesting fats, proteins and carbohydrates, and hormones for regulating blood glucose levels. The portion of the pancreas responsible for producing digestive enzymes is called the exocrine portion and the hormone producing part is called endocrine. Due to the presence of both endocrine and exocrine glandular tissue, it is classified as heterocrine gland. The endocrine portion of pancreas is composed of two types of cells, namely alpha cells for producing the hormone glucagon and beta cells for producing the hormone insulin. Glucagon stimulates the liver to produce glucose from glycogen in the event of decreased blood glucose levels. Whereas, insulin is responsible for decreasing blood glucose levels by stimulating the liver to store glucose in the form of glycogen.
Diabetes Type 3c (T3cDM)
In the events of chronic pancreatitis, pancreatic cancer [1], pancreatic trauma, cystic fibrosis, fibro calculous pancreatopathy,[2] or resection of pancreas, the beta cells of the endocrine portion of the gland can become dysfunctional. There is inadequate production of digestive enzymes and insulin from the pancreas, leading to poor glycemic control. This type of secondary diabetes, arising due to diseases of the exocrine portion of the pancreas is termed as type 3c diabetes or pancreatogenic diabetes by the American Diabetes Association (ADA) [3] and World Health Organization (WHO).[4]
Due to lack of information, most of the doctors diagnose type 3c diabetes as type II diabetes, having life threatening repercussions. Treatment for a person having type 3c diabetes involves insulin administration whereas anti-glycemic drugs are prescribed for managing type II diabetes. If immediate insulin is not made available to the patient, it can damage the eyes, nerves and kidneys. [5] Almost 90% of the cases of diabetes arising out of diseases of the exocrine portion of the pancreas are misdiagnosed as type II diabetes. This mis-diagnosis clearly flags the issue that wrong diagnosis leads to lower quality care.
Higher mean HbA1c levels and poorer glycemic control was observed in people with type 3c diabetes. The requirement of insulin is markedly higher in these patients.
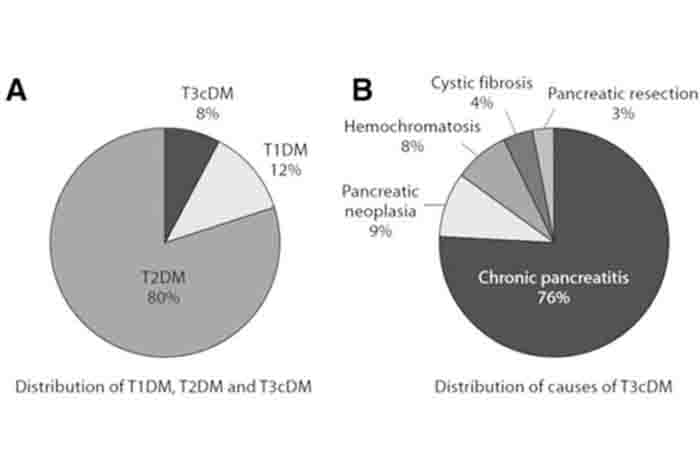
Estimated Prevalence of Type 3c Diabetes
The exact prevalence of type 3c diabetes in the world is not known but it can be estimated by determining the number of cases of pancreatic diseases reported globally. Until proper statistics are available, the researchers suggest that to assume that 1-9% of all the diabetic people in the world have type 3c diabetes. [6]
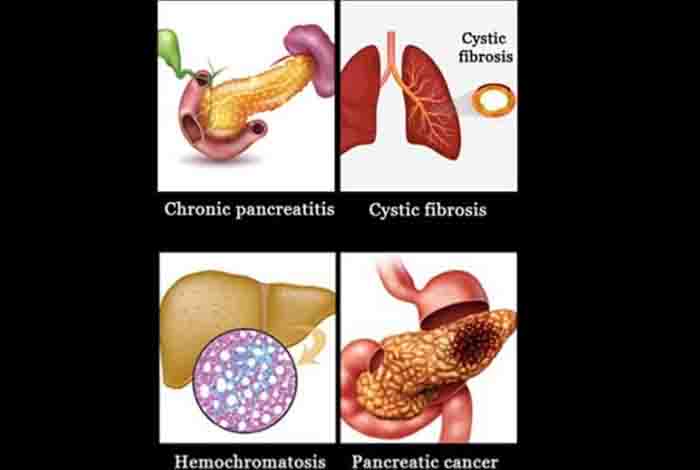
Causes of Type 3c Diabetes
Type 3c diabetes is a form of secondary diabetes which occurs when the exocrine portion of the pancreas gets severely affected. Some of the diseases that can result in type 3c diabetes are:
- Acute, relapsing or chronic pancreatitis
- Pancreatectomy
- Trauma to pancreas
- Pancreatic cancer
- Cystic fibrosis
- Hemochromatosis
- Fibrocalculous pancreatopathy
Except for pancreatic cancer, the damage to the pancreas should be extensive for type3c diabetes to occur.
When the exocrine portion of the pancreas gets affected, the complicated cycle of nutrient digestion, absorption and utilization gets affected at various levels. Improper digestion and malabsorption of nutrients are accompanied with some degree of exocrine dysfunction, in which there occurs deficiency of glucagon, insulin, pancreatic peptides and incretin hormones. [7] All these irregularities lead to fluctuating blood glucose levels and hypoglycemic reaction, which includes shakiness, sweating, anxiety, rapid heartbeat, hunger, nausea, confusion and irritation.
Diagnostic Criteria for Type 3c Diabetes
Since the disease is so new, there are no proper diagnostic criteria for type 3c diabetes. However, some features can be used for identifying type3c diabetes. These are:
- Exocrine pancreatic insufficiency
- Pancreatic abnormality on imaging
- Absence of auto-immune markers of type I diabetes
- Impaired beta cell function
- Absence of insulin resistance
- Impaired secretion of incretins
- Low serum concentrations of lipid soluble vitamins like A,D,E,K
- Advanced destruction or surgical removal of pancreas [8]
Management of Type3c Diabetes
At present, no specific guidelines are available to manage type3c diabetes as a separate entity. However, a few steps might be taken to keep the blood glucose levels under check.
1. Glycemic Control
The main focus of a physician treating a patient with type3c diabetes is to maintain HbA1c levels >7%. HbA1c is a marker that is commonly used for measuring long term glucose levels in the blood. Hb or hemoglobin is a protein found in red blood cells that helps in carrying oxygen from the lungs to different parts of body. This protein, after binding with glucose become glycated and is referred to as glycated hemoglobin, denoted as HbA1c. By measuring the HbA1c levels in the body, clinicians are able to determine the average blood glucose levels for a long period of time. If the body’s blood glucose levels have been high in the past few weeks, its HbA1c levels would also be high. Therefore, it is important to keep HbA1c levels within normal limits.
In people with type3c diabetes, there is also a chance of development of ‘brittle diabetes or Labile Diabetes’, that refers to a particularly hard to manage type I diabetes. People with type 3c diabetes might also begin to display the symptoms of brittle diabetes- frequent and extreme swings in blood glucose levels, causing hyperglycemia or hypoglycemia.
Symptoms of brittle diabetes when the blood glucose levels are extremely low are
- Anxiety
- Sweating and chills
- Irritability
- Dizziness
- Nausea
- Blurred vision
- Shakiness
- Confusion
- Headache
- Seizures
- Unconsciousness
Symptoms of brittle diabetes when blood glucose levels are low are
- Frequent urination
- Blurred vision
- Extreme thirst
- Fatigue
- Headache
Therefore, while treating a patient with type 3c diabetes it is extremely important to avoid hypoglycemia as it can lead to breathing trouble, weakness, confusion, abdominal pain and in severe cases, coma.
2. Lifestyle Modifications for Managing Type3c Diabetes
Certain changes in lifestyles can help in managing the disease affecting the exocrine portion of the pancreas as well as type 3c diabetes. Complete abstinence from alcohol and smoking is extremely important, as both of these habits can cause an increase in pancreatic inflammation and fibrosis and cause pain. Alcohol also helps in inhibiting hepatic glucose production and hence can lead to hypoglycemic conditions in the body. Therefore, abstinence from alcohol is also recommended for managing type3c diabetes. It is also suggested to indulge in moderate aerobic exercise for at least 150 minutes per week.
3. Nutrition
People having type3c diabetes should take precautions to prevent/ treat malnutrition and minimize meal induced hyperglycemia. Following points should be kept in mind while planning the meals for a type 3c diabetes patient:
- Meals rich in soluble fiber and low in fat should be encouraged
- Vitamin D rich diet
- Well-balanced diet
- Fat soluble vitamins should be supplemented by the diet
- No restriction on salt and protein intake
4. Anti-Hyperglycemic Agents
Different treatment options should be selected for managing the symptoms of type3c diabetes.
In people with chronic pancreatitis-associated diabetes with mild hyperglycemia, or hypoglycemic agents can be prescribed. Metformin can be prescribed for decreasing the risk of pancreatic cancer, but it is often tolerated badly in pancreatitis patients. Even thiazolidinediones are not given to such patients. Insulin secretagogues like sulfonylureas and glinides also increase the risks of cancer and hypoglycemia. No data is available for use of potential sodium glucose cotransporter 2 inhibitors in these patients.
Insulin is known to increase the risk of cancer but in majority of these patients, insulin is the preferred choice of treatment for managing blood glucose levels. Insulin use has shown to improve lung function, nutritional status, blood glucose control and decreased mortality.
5. Promising Novel Drugs
Pancreatic peptide (PP) is showing promising outcomes for treating type 3c diabetes occurring due to chronic pancreatitis. It helps in increasing the expression of insulin receptors in the liver and therefore enables effective utilization of insulin that is circulating in the body.
6. Surgery
In some patients with serious complications like recurrent acute and chronic pancreatitis, a surgical procedure known as total pancreatectomy with islet auto transplantation is performed. It helps in reducing frequent hospitalizations and the risk of severe diabetes mellitus. It is also helpful in people who are at a high risk of developing pancreatic cancer.
Prevention of Type 3c Diabetes
By reducing the risk factors that lead to pancreatitis, pancreatogenic diabetes can be prevented. These are:
- Reduce alcohol consumption
- Avoid smoking
- Reduce chances of developing gallstones
- Follow a healthy diet rich in fresh fruits and vegetables
- Exercise regularly
- Avoid obesity
Conclusion
The need of the hour is to correctly diagnose the type of the diabetes and to fund research for type 3c diabetes. Knowledge gaps can become fatal for the patient having type3c diabetes. There is a need to develop validated diagnostic criteria and treatment regimens. It is also required to estimate the prevalence of this disease in the world and educate health care professionals about this disease.