Overview and Facts
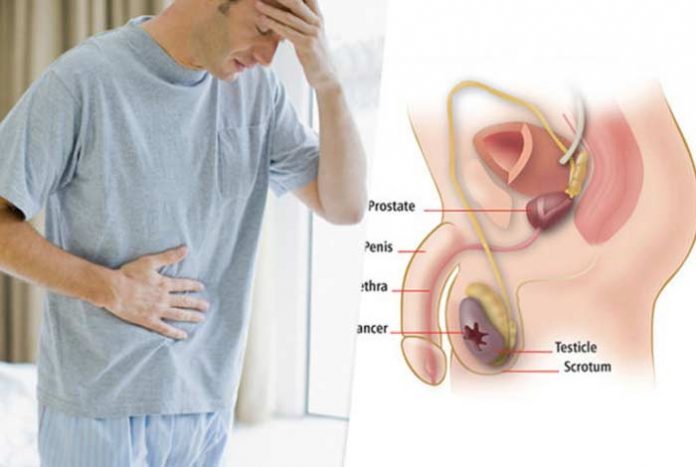
Testicular cancer is a type of cancer that gets formed in the testicles. It is a condition that develops when cells in the testicles, known as testicular cells become abnormal or malignant in one or both the testicles. It is a highly common type of cancer in men, who are in the age bracket of 15-44 years. However, when compared with other types of cancer, testicular cancer is rare.
Testicles are two egg-shaped glands present inside the scrotum – loose skin present directly below the penis. Testicles are present in the scrotum and held together by spermatic cord. The testicles are male sex glands that produce testosterone and sperm. Almost all testicular cancers originate in the germ cells. The cells that make sperm are known as germ cells. Most testicular cancers start as one of the two types of germ cell tumors, namely seminoma or non-seminoma. Another type of this cancer is stromal tumor. Additionally, there are secondary tumors that spread to the testicles from other parts of the body.
In 2016, approximately 8,850 men in the U.S. were diagnosed with testicular cancer. The average age of diagnosis is 33 years. Around 7% of the cases are diagnosed in men, who are 55 years or older and nearly 7% of the cases get diagnosed in young boys (in their adolescent years). In the past 40 years, the number of cases of testicular cancer have increased. However, death rates due to testicular cancer are on the fall.
It has been predicted that around 410 men die each year due to testicular cancer. These deaths are from cancers that spread from the testicles to other body parts and could not be treated with surgery, chemotherapy, radiation therapy or other types of treatments. The five-year survival rate for men with testicular cancer is 95%. This means 95 out of 100 men will survive at least 5 years after the cancer has been detected.
The rates of survival are higher in men, who have been diagnosed with early-stage cancer. Survival rates are not very impressive for those, who have been diagnosed with late-stage cancer. For men in whom the cancer has not spread beyond the testicles, the survival rate is 99%. The rate of diagnosis of the condition at this stage is 68%. For men in whom the cancer has been spread to the lymph nodes in the back of the abdomen, the rate of survival is 96%. In those men in whom the cancer has spread beyond the abdominal lymph nodes, outside the testicles, the survival rate is 73%. Around 11% of testicular cancers are diagnosed at this stage.
Testicular cancer is rare and there are as less as 4 out of 1000 chances of developing this condition. In almost 90% of the cases, testicular cancer is present as a lump in the testicle. It is generally more common in Caucasian males as compared to African or Asian men.
Types and Symptoms of Testicular Cancer
Types of Testicular Cancer:
There are two main types of testicular cancer:
- Seminoma
- Non-seminoma
1. Seminoma: These grow and spread slowly as compared to non-seminomas. These are further divided into two types: classical seminomas and spermatocytic seminomas. These can be distinguished on the basis of their appearance under the microscope.
- Classical Seminomas: Around 95% seminomas are classical. They occur in the men in the age group of 25 to 45.
- Spermatocytic Seminoma: It generally occurs in older men. The average age at which it is diagnosed is 65 years. The likelihood of these tumors spreading to other parts of the body is less in this case as compared to classical seminomas.
Some seminomas are known to increase the levels of protein in the blood, known as human chorionic gonadotropin (HCG). HCG can be diagnosed with a blood test.
2. Non-Seminomas: These types of germ cells tumors are generally found in men in their late twenties and early thirties. There are further four subdivisions of this type of cancer. These are listed below:
- Embryonal carcinoma
- Yolk sac carcinoma
- Choriocarcinoma
- Teratoma
Most of the testicular cancers are a combination of different types, i.e., mix of seminoma and non-seminomas.
- Embryonal Carcinoma: This non-seminoma cancer occurs in nearly 40% of testicular tumors. In the pure form, i.e., without any combination with others, it occurs in 3-4% of the cases. These tend to grow quickly and spread outside the testicles.
- Yolk Sac Carcinoma: These are so called because these cells resemble yolk sac of early human embryo in their appearance. This is quite a common form of cancer, particularly in children (infants), but pure yolk sac carcinomas are rare in adults. In children, these can be operated successfully. However, pure form of occurrence of this type in adults is a matter of concern. Yolk sac carcinoma respond pretty well to chemotherapy.
- Choriocarcinoma: It is a rare and strong type of testicular cancer in adults. In its pure form, there is likelihood of spreading of this cancer to other organs, like lungs, brain and bones. This also increases blood levels of HCG.
- Teratoma: These are germ cell tumors that look like the layers of a developing embryo: endoderm (innermost layer), mesoderm (middle layer), ectoderm (outer layer). There are three main types of teratoma— Mature Teratoma, Immature Teratoma, Teratoma with somatic type malignancy.
Other types of testicular cancer include:
- Stromal Tumors: These develop in stroma of the testicles. These tumors are known as gonadal stromal tumors. They contribute to about 5% adult testicular tumors and 20% of childhood testicular tumors. It is further divided into two types: Leydig cell tumors and Sertoli cell tumors.
- Secondary Testicular Cancer: Cancers that start in some other organ and then metastasize to the testicles are secondary testicular cancers Lymphoma is the most common secondary testicular cancer. In young boys with leukemia, the leukemia cells can form a tumor in the testicles. This is also an example of testicular cancer.

Symptoms of Testicular Cancer:
Some common symptoms of testicular cancer are discussed below:
- Lump formation or swelling, generally not accompanied with pain, is found on either side of the testicle. When detected early, it may be about a size of a marble, but don’t think it cannot grow much larger than this.
- Pain or swelling in the testicles in the scrotum
- Feelings of heaviness in the scrotum. For example, one testicle may feel heavier or firmer than the other
- Feeling of ache in the groin or abdominal area
- Building up of fluid in the scrotum
- Pain in back, breath shortness, pain in chest
- Growth of breast and tenderness. Some testicular tumors produce hormones causing tenderness of breast or growth of breast tissue.
- Swelling in legs. Developing a blood clot may be one of the first signs of testicular cancer
- Change in size or formation of lump in testicles
- Cyst formation in epididymis (epididymis is a tube that connects testicles to the duct in the reproductive system)
- Pain, feeling of injury or twisting
- Enlarged or swollen lymph nodes

Risk Factors of Testicular Cancer
Several risk factors associated of Testicular Cancer are as follows:
- Undescended Testicle: This means either one or both the testicles are unable to move from the abdomen into the scrotum before birth. Males with this condition have high likelihood of having testicular cancer than those with normally descended testicles. Normally, the testicles develop in the abdomen of the fetus and move down into the scrotum before birth. In around 3% of the boys, testicles do not go down in the scrotum before birth. The risk of testicular cancer is higher in such boys or men.
- Family History: Testicular cancer runs in families. If someone has a father or brother with testicular cancer, the chances for him to get the disease also increases. However, there are many men, who have testicular cancer, but do not have anyone in the family with testicular cancer.
- HIV Infection: Men with HIV or AIDS are at an increased risk of developing testicular cancer. There are not many known infections that increase risk of testicular cancer.
- Cancer in the Other Testicle: If there is cancer in one testicle, the likelihood of it to develop in the other testicle increases. So, it can be a risk factor.
- Age: More than 50% of testicular cancer occurs in the men aged 15-44. However, it can affect men of any age.
- Race and Ethnicity: The chances of the development of testicular cancer in White men is 4 to 5 times more than in Asian American and Black men. The exact reasons for this difference is not known. The risk is more in men in the U.S. and Europe and lowest in those residing in Africa or Asia.
- Body Size: Some studies have revealed that men, who are taller have greater chances of having testicular cancer. Studies need to be conducted to explain a relation between testicular cancer and body weight.

Do I have Testicular Cancer?
Simply having lumps on one or both of the testicles does not mean that one has testicular cancer. Some lumps are caused by noncancerous or benign conditions. These, generally, do not require any treatment. But, it is always advised to see a doctor to examine changes in the testicles like swelling and lump formation. Sometimes an epididymal cyst forms when the long tube present at the back of testicles, called epididymis gets filled with fluid and is unable to drain. This type of testicular lump is quite common. This is not testicular cancer and it heals on its own; hence, should not be a cause of worry.

Causes and Prevention of Testicular Cancer
Causes of Testicular Cancer:
The exact cause of testicular cancer is not known. It is believed that testicular cancer occurs when healthy cells become malignant or get altered. Healthy cells grow and divide in orderly fashion, so that the body works properly. But sometimes, these cells grow out of control and develop abnormalities and carry on the process of division even when there is no requirement of new cells. These cells form a mass in the testicle. The uncontrolled cell division can also invade the blood stream and lymph system, and can metastasize to other body parts. This results in testicular cancer.
Prevention of Testicular Cancer:
Prevention is adoption of methods that are used to prevent even other types of cancer and not just testicular cancer. These steps may include:
- Removal of toxins from the body and environment that are a cause for most types of cancer
- Eating healthy diet that boosts the immune system and fights cancer also helps. Unhealthy foods should be avoided at all costs.
- Making healthy lifestyle choices along with incorporating physical exercises and stress management activities in one’s daily life. Also ensuring that daily optimum nutrition requirements are met through diet or supplements.
- Liver must be cleansed and protected as it is a vital organ that plays an important part in the removal of toxins. It has been observed by Max Gerson, a noted German physician, that in nearly all cases of cancer, liver is impaired.

Diagnosis and Tests of Testicular Cancer
The doctor may physically examine the testicles for swelling and tenderness as well as to locate the lumps. He may also examine the patient’s abdomen and other parts of the body like lymph nodes to detect possible signs of cancer. If there is lump formation, testing needs to be done. Some tests for testicular cancer detection are listed below:
- Ultrasound of the Testicles: If a doctor suspects testicular cancer, the first test that he may suggest is ultrasound. Sound waves are used in this test that create images of the internal organs. If it is a solid lump, it is more likely to be cancer. So, further tests are required or sometimes even surgery to remove the testicle. Ultrasound is a test that does not use radiation. Patient is asked to lie on the back while a transducer is moved along the skin of the scrotum.
- Blood Tests: There are several blood tests that can detect tumors of the testicles. When a male has testicular cancer, there are high levels of certain proteins, called tumor markers like HCG and AFP (alpha-fetoprotein). If these tumor markers are present in the blood, it signifies testicular cancer. Increase in AFP and HCG levels can also tell which type of testicular cancer it is. Non-seminomas generally increase AFP and/or HCG levels. Pure seminomas sometimes raise HCG level, but they never raise AFP levels.
- Biopsy: Many types of cancer are detected by removing a small part of the tumor and looking at it under the microscope. This procedure is known as biopsy. Biopsies are generally not done for testicular tumor as it has risk of spreading the cancer to other body parts. The doctor can get an idea whether it is testicular cancer based on results of ultrasound and blood tumor markers.
- Imaging Tests: Imaging tests use magnetic fields, X-ray and radioactive substances to create a picture of what is inside the body. Ultrasound is also a type of imaging test. These tests can be done to understand whether treatment has worked, how far cancer has spread, and if there is any chance of cancer coming back after the treatment.
- Computed Tomography (CT) Scan: CT scans can be used to determine the stage of the cancer by depicting if it has metastasized to other organs like lymph nodes, lungs and liver. CT scans are also used for guiding a biopsy needle in the area, where the cancer has spread.
- Magnetic Resonance Imaging (MRI): MRI scans help look at brain and spinal cord. This is done in patients with testicular cancer if the doctor thinks that cancer might have spread to these areas. MRI makes use of radio waves and strong magnets in place of X-rays.
- Positron Emission tomography (PET) Scan:These scans can help locate cancer cells in the body. It also makes sense to see if lymph nodes that are enlarged after chemotherapy have cancer. PET scans are more useful in case of seminomas as compared to non-seminomas. These are therefore not very often used in patients with non-seminoma.
- Bone Scan: A bone scan helps spot if cancer has spread to the bones. During this test, a small amount of radioactive material is injected into a vein. The areas of active bone changes may suggest metastatic cancer, but arthritis and other bone diseases may also be the reason.

Treatment and Care for Testicular Cancer
Treatment of Testicular Cancer:
There are different treatment options available for testicular cancer like chemotherapy, surgery and radiotherapy. However, the treatment plan depends on the type of testicular cancer that one has, and also, on the stage of the condition.
The first line of treatment for testicular cancer, irrespective of the stage is, to surgically remove the testicle, which has the cancer. This process is known as orchidectomy.
After removal of affected testicle in stage one seminoma, a single shot of chemotherapy may be given to prevent cancer to return. Radiotherapy course is also recommended. Further treatment after surgical removal is only needed in those cases, in which there is chance of recurrence. For testicular cancer in stage two, three and four, approximately three to four cycles of chemotherapy may be given with a combination of different medications.
- Orchidectomy: It is a surgical procedure for the removal of testicle. If one has testicular cancer, the whole of affected testicle may need to be removed surgically. Only removing the tumor may allow the cancer to return, thus increasing the chances of recurrence. When the entire testicle is removed, the chances of achieving full recovery is higher. This will also not have a negative effect on a person’s sex life. Around 2% of the people get a testicular cancer in the remaining testicle after having it in one testicle. If detected in early stages, orchidectomy is the best treatment for testicular cancer.
- Surgery of the Lungs and Lymph Nodes: Advanced cases of testicular cancer may spread to lymph nodes. The surgery of lymph nodes is carried out under general anesthesia. Laparoscopic retroperitoneal lymph node dissection is a type of surgery performed to remove the lymph nodes. During this surgery, a surgeon makes incisions or cuts into the patient’s abdomen. An instrument, known as endoscope is inserted in the abdomen through the incision. Surgical instruments are sent down the endoscope and can be used to remove the lymph nodes.
- Radiotherapy: This technique uses high-energy radiation beams for destroying the cancer cells. Seminomas may sometimes require radiotherapy post-surgery to prevent the cancer from coming back. Radiotherapy is also used in cases when the patient is not able to tolerate the complex chemotherapies used for the treatment of stage two, three and four testicular cancer.
- Chemotherapy: In this technique, medicines are used to kill the malignant or cancerous cells in the body in order to stop them from multiplying. Chemotherapy may be required in case of advanced testicular cancer or if the cancer has spread to other parts of the body. Chemotherapy medicines are generally injected in the vein. Chemotherapy can have side effects also.
Caring for People with Testicular Cancer:
Testicular cancer and its treatment have several side effects. Not only is treatment important, but also an crucial part of the cancer care is to relieve a person of its symptoms and side effects. This is known as palliative care, which is associated with supporting the patient in all aspects that is physical, social and emotional. Palliative care varies widely and includes medication, changes in nutrition, emotional support, relaxation technique and other therapies. Doctor must be consulted by the patient and family to understand the goals of the treatment. They must be made aware of the side effects of the treatment plan.

OTC Medications and Self-Management Methods for Testicular Cancer
OTC Medications for Testicular Cancer:
Nonsteroidal, anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen for relieving pain can be taken by the patient. These are available over the counter (OTC). However, other medicines must be consumed only after a qualified practitioner has prescribed the medication.
Self-Management Methods for Testicular Cancer:
Self-examining the testicles regularly for any lump or swelling is important as far as identification of testicular cancer is concerned in order to detect it in its early stages. A monthly testicular self-examination may be conducted to identify testicular cancer early.
A person can examine his testicles after a warm bath or shower. The warm water will relax the skin of the scrotum, making it easier to feel any lump or something unusual. One can use both hands for examining the testicles. Index and middle fingers should be placed below the testicles and thumb should be placed on top. After this one should roll the testicles in hands.
A person may feel different sizes of testicles, which is normal. While examining the testicles, one may find a cord like structure on the back of the testicles. This is epididymis, which stores and transports sperms. This should not be confused with a lump. Look out for any lump, which can be quite large in size. Notice the change in size and shape of the testicles.

Natural Ways to Cure Testicular Cancer
Some common ways to prevent and manage testicular cancer naturally are discussed below:
- Basil: It contains antioxidants that prevent the development of cancer. Basil leaves are known to be beneficial in testicular cancer as it prevents the recurrence of cancer in the body.
- Allylic Sulfide: It has anti-cancerous properties. It is present in vegetables, garlic and onions. Allylic sulfides also have antibiotic and antifungal properties. It is considered as a potent natural ingredient to manage testicular cancer as it is rich in allylic sulfide.
- Berries: They are rich in bioflavonoid. These can be considered as natural cure for testicular cancer as these have anti-cancerous effects and properties.
- Strawberries: These have ellagic acid, which is useful in fighting cancer. They protect from the damage of genetic material by carcinogens.
- Green Tea: These contain polyphenols and flavonoids that help protect against cancer as these have anti-cancerous properties. Drinking at least two cups of green tea a day fulfill the requirement of flavonoids by the body.
- Turmeric: Turmeric contains curcumin, which is used in the prevention and cure of testicular cancer. It further protects the liver from damage by various factors.
- Broccoli: This contains compounds that have anti-cancerous properties. Liver detoxification is also improved with daily consumption of broccoli.
- Mustard: It contains isothiocyanates that prevent the development of cancer in the body.
- Tomatoes: It is rich in lycopene, which has anti-cancerous properties. Eating around one serving of tomato per week cuts the risk of testicular cancer by about 60%.
- Carrots: These are rich in beta carotene. Beta carotene has anti-oxidant and anti-cancerous effects.
- Green Peas: It contains compounds that have cancer-fighting potential. They also help fight macular degeneration.
- Naturopathic Medications: Naturopathic therapies to manage testicular as well as other types of cancer include herbal and botanical preparations, exercise, yoga, dietary supplements, acupuncture and chiropractic.

Health Tip by Expert
Practicing healthy habits like eating a diet which is balanced and getting proper sleep and incorporating exercise schedule in the daily routine can help control symptoms of testicular cancer.




