
Overview and Statistical Facts of Cholera
Food and water are the most important things for survival after air. But these life-giving boons can become a bane when they get contaminated and cause serious diseases. One such disease is a potentially fatal, intestinal diarrhea, caused due to a bacterial infection, known as Cholera. The bacterium responsible for causing this disease is Vibrio cholerae, which is shed off from the body of an infected person through feces. When these feces come in contact with water, they contaminate it and consumption of drinks and food items made from this contaminated water can cause cholera in a healthy person. This disease is known to affect only humans and no other animal.
Cholera is often termed as a disease of inequality as its incidence is extremely rare in developed countries but is still a major health concern in the developing and underdeveloped world. The disease can be endemic, pandemic or epidemic. Cholera usually presents itself in a mild form or without symptoms but can become severe in nearly 5-10% cases. It can become fatal within hours due to excessive dehydration if immediate treatment is not made available, even in individuals who were previously healthy.
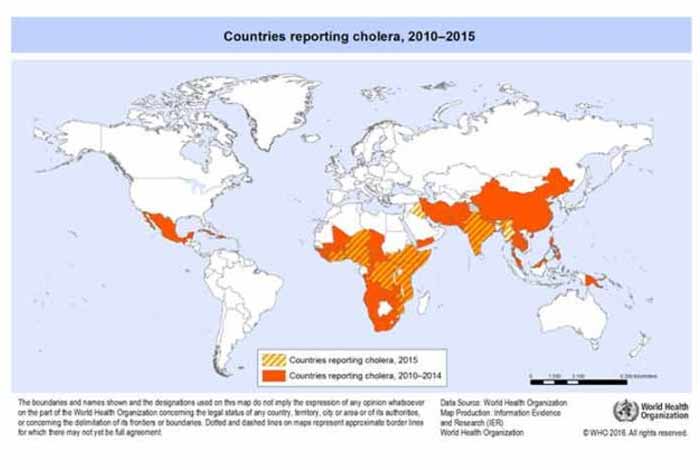
According to WHO, the cholera map of the world overlaps with the global poverty map. This is due to lack of modern sewage and water treatment facilities in the developing and underdeveloped countries. When poverty, natural disasters or war forces people to live in crowded areas without proper sanitation, the chances of cholera outbreaks increase.
According to a WHO report, each year, 1.3 million to 4.0 million cases of cholera are reported worldwide, out of which 2100 to 143000 cases result in death. In order to reduce the number of deaths due to cholera by 90%, a global strategy has been launched by WHO in 2017. [1]
The disease can be easily treated and death from dehydration can be prevented by using an inexpensive and simple rehydration solution.
Types and Symptoms of Cholera
Types of Cholera
There are two types of cholera, namely:
- Classic cholera: It is the most common form of cholera in which large quantities of fluid is lost from the body in a very short period of time.
- Cholera sicca: It is a rare form of cholera in which the fluids get withdrawn from the body but are not secreted out. Rather, they are stored in the digestive tract.
Symptoms of Cholera
Cholera remains asymptomatic or mild in most of the people infected with the bacteria and they do not even realize they have been infected. However, they continue to shed the bacteria in their stools for 7 to 14 days after the infection subsides, which can contaminate water and infect others in the absence of proper sanitation facilities. Even if cholera produces symptoms, it is often so mild or moderate that it is difficult to distinguish it from diarrhea caused due to other reasons. Serious signs and symptoms develop only in 1 out of 10 patients, usually few days after being exposed to the bacteria.
Following are the symptoms observed in a cholera patient:
a. Diarrhea: In cholera, diarrhea appears suddenly and within a few hours, the amount of fluid loss from the body can become dangerous. It has a characteristic pale, milky appearance that resembles the water in which rice has been washed and is called rice water stool.
b. Nausea and Vomiting: In the early stages of the disease, the patient might experience vomiting for several hours.
c. Dehydration: It is the most serious complication of this disease and it can develop within a few hours of the onset of symptoms. It can range from mild to severe, depending on the amount of body fluids lost. If the fluid loss is 10% or more of the total body weight, it indicates severe dehydration, which can become fatal if left untreated.
Dehydration also causes a rapid loss of minerals from the blood which maintain the fluid balance in the body, resulting in a condition called electrolyte imbalance.
Electrolyte imbalance can lead to following serious conditions;
- Muscle cramps due to loss of sodium, potassium, and chloride
- Shock, due to decreased blood pressure and oxygen levels in the brain from severe fluid loss.
- Death, in case of severe hypovolemic shock.
Symptoms of dehydration include:
- Irritability
- Lethargy
- Dry mouth
- Sunken eyes
- Extreme thirst
- Dry and shriveled skin which is slow to bounce back on folding
- Little or no urine output
- Low blood pressure
- Irregular heartbeat
If cholera develops in children, the signs and symptoms are the same as those observed in adults. However, they are more susceptible to dehydration and might develop:
- Altered state of consciousness
- Seizures
- Coma

Risk Factors of Cholera
Consumption of foods or drinks made from water that has not been treated to eliminate the risk of contracting V. cholerae in areas where cholera is common can cause the disease. Cholera outbreaks occur where sanitation is compromised due to poverty, natural disasters or war, forcing people to live in crowded areas. In countries where hunger is a major problem, people consume contaminated food and water in order to satiate themselves, thereby increasing their chances of contracting cholera. In the developed countries, where proper sanitation facilities occur and hunger is not a major issue, cholera is almost absent. Only travelers visiting developing and underdeveloped countries develop cholera, if they consume contaminated food and water.
Some of the major risk factors that contribute to developing cholera are:
1. Having improper sanitation facilities which can contaminate food and water
2. Having low stomach acid which decreases the body’s ability to fight infection
3. Being in close contact with cholera patient
4. Consuming raw or poorly cooked shellfish
5. Visiting rural and impoverished regions
6. Working in hospitals
7. Being in the age group of 2-4 years
8. Having a weak immune system
9. Having blood type O
10. Taking medicines to reduce stomach acid, like pantoprazole and other H2 blockers
11. Living in areas hit by natural disaster, war and poverty

Do I Have Cholera?
If you experience severe diarrhea that appears suddenly and is pale and milky, like rice water, chances are you have cholera. Along with diarrhea, you may also experience nausea and vomiting that may persist for several hours. Extreme thirst, lethargy, muscle cramps and sudden drop in body weight are all symptoms of dehydration caused due to cholera.
These symptoms are also observed in cases of food poisoning, dehydration and diarrhea occurring due to reasons other than cholera. Consult your doctor immediately and start oral rehydration solution as dehydration can become serious very quickly.
Causes and Prevention of Cholera
Causes
Cholera is caused by the bacterium, Vibrio cholerae, which spreads through the fecal-oral route. On consuming foods and drinks made from water contaminated with Vibrio cholerae, a person can develop cholera. Nearly 100 million bacteria are required to infect a healthy individual and hence a significant amount of contamination is required in order to develop the infection. Transmission of disease from direct contact is rare except during outbreaks. At the time of epidemic, the bacteria becomes extremely contagious and infects more people due to widespread contamination of food and water.
Bacteria causing cholera, after entering the human body, are killed in the extremely acidic environment present in the stomach. The few surviving bacteria reach the small intestine and start producing toxins. This causes diarrhea, which carries a number of multiplying bacteria with it. If proper sanitation practices are not followed, it can contaminate the water and cause infection in other people on consumption.
Consuming foods and drinks prepared from contaminated water can help in spreading cholera. If improperly treated sewage water is used for irrigating fields, the bacteria can contaminate the crops and cause infection in people who consume these crops. Eating raw or poorly cooked seafood, especially shellfish growing in naturally contaminated water can cause cholera. These bacteria also survive in natural water sources, surviving either by itself or by interacting with zooplankton, phytoplankton and others. Consuming such water can also cause cholera, even without any prior contamination with fecal matter of a diseased person.

Prevention:
Following steps might be taken for preventing cholera:
1. Frequent washing of hands: Wash your hands frequently using water and soap. Rub your hands together for at least 15 seconds before rinsing. Always carry an alcohol-based hand sanitizer, in case there is an unavailability of water.
2. Drink treated water: Always opt for bottled waters or treated water. Even if buying bottled waters, make sure to wipe the outside of the bottle before you open the cap. Also, avoid ice in your drinks.
3. Eat properly cooked and hot foods: Always consume food that is cooked in front of you and served hot.
4. Do not consume foods that are improperly cooked like Sushi.
5. Do not consume fruits and vegetables that have been cut for a long time. Rather, consume fruits that you can peel off yourself.
6. Beware of dairy products like ice-cream and unpasteurized milk.
7. Vaccinate yourself before traveling to cholera endemic regions.
8. Work as a community to eliminate any stagnant water near you and adopt modern sanitation practices.
9. Avoid consumption of shellfish
Cholera vaccine:
When traveling to a cholera affected area, you can get yourself vaccinated with cholera vaccine. This vaccine contains small doses of live attenuated cholera bacteria that on reaching the gut get replicated and activate the immune system in order to build immunity against the bacteria. Later, when the body comes in contact with cholera bacteria, the immune system is able to protect the body against the disease.
Ten days before traveling to a cholera affected region, vaccination against the disease can be taken. The vaccine is available as a single, oral liquid dose or as double dose oral vaccine, which contains inactivated or non-live cholera bacteria. These double dose vaccines, although being WHO pre-qualified, are not available in the U.S. The U.S.A. FDA has only approved the single dose vaccine which is especially beneficial if the person is visiting cholera affected region on a short notice.
Complete protection is not guaranteed by the cholera vaccine and should never replace the standard prevention and control measures.
Diagnosis and Tests for Cholera
Although signs and symptoms of severe cholera are unmistakable in endemic areas, the only way to confirm a diagnosis is to identify the bacteria in a stool sample.
A caregiver performs the primary examination and records the medical history of the person showing symptoms. Characteristic rice water appearance of stools, especially if there has been a local outbreak of cholera recently, usually confirms the diagnosis of cholera.
Microscopic evaluation of diarrhea of patient can be done and if it reveals a mobile, comma shaped bacteria, Vibrio cholerae, cholera is confirmed. While confirming cholera, definitive tests for diagnosing other diseases which also can cause dysentery are also performed. Treatment is usually started before cholera is confirmed in order to prevent dehydration.
In order to assist health care givers in remote areas, rapid cholera dipstick tests have now been made available which help in early detection of cholera. Early identification of disease aids in prompt treatment. This can help in bringing down the number of deaths occurring due to cholera substantially and public interventions can be started earlier to prevent epidemic.

Treatment and Care for Cholera
Treatment:
Rehydration is the most important step in treating cholera. It is achieved in two steps: rehydration and maintenance. Achieving the normal hydration states is the primary objective of rehydration, which nearly takes 4 hours. This can be achieved by replacing the ongoing loss of fluids due to diarrhea. This step is called rehydration. Next priority is to maintain the normal state of hydration, which comprises the maintenance phase.
Oral route is generally favored for re-hydrating and maintaining the normal hydration state unless the symptoms turn severe. Recommendations have been laid down by WHO for replacing fluids in the patients. WHO and UNICEF have made extensive efforts for making oral rehydration solution (ORS) readily available over-the-counter in pharmacies in most of the countries across the globe. Potassium, glucose and bicarbonate levels in the body are replenished by taking ORS. Regular monitoring of body fluids is required by the patients and they are kept under strict observation until diarrhea stops or becomes infrequent and small in volume.
Symptoms of cholera can also be managed by using antibiotics. However, according to the guidelines laid down by WHO, it should only be used as an adjunct to rehydration therapy. Antibiotics can help in bringing down the volume of diarrhea in severe cases and the time for which bacteria is shed off from the body of the diseased person. Antibiotics help in putting a stop on the diarrhea within 48 hours, thereby decreasing the time of hospital stay. Anti-diarrheal medicines should never be given for managing the symptoms of cholera. If possible, antibiotics should be given only after identifying the strain of cholera bacteria for providing an effective treatment while avoiding the risk of developing drug-resistant strains.
A case of cholera that is untreated can cause death within hours. So, it is important to provide immediate medical care to the afflicted individual. Antibiotics belonging to classes such as tetracycline, fluroquinolone, cotrimazole, cholarmphenicol macrolides and penicillin are used for treating cholera. They are described below:
A. Fluoroquinolones : These drugs inhibit the enzymes topoisomerase IV and topoisomerase II (DNA gyrase) found in the bacteria, which help them in multiplication. By inhibiting these enzymes, bacterial multiplication is stopped.
Examples: Ciprofloxacin and norfloxacin
B. Tetracyclines: These drugs are stop bacteria from multiplying and are bacteriostatic in nature. They work by inhibiting the synthesis of protein in the bacteria and prevent their multiplication.
Examples: doxycycline hyclate, tetracycline hydrochoride, minocycline hydrochloride
C. Macrolides: These drugs prevent synthesis of protein in bacteria and inhibit their multiplication in the body. However, they do not kill the bacteria and their action is termed as bacteriostatic.
Examples: azithromycin
D. Aminopenicillins: An enzyme, known as transpeptidase is required by the bacteria for the synthesis of its cell wall. Aminopenicillins inhibit the enzyme and therefore, bacterial cell wall synthesis is stopped. This prevents bacterial multiplication in the body.
Example: ampicillin sodium
E. Cotrimoxazole: Trimethoprim and sulphamethoxazole, in a fixed dose combination are two antibiotics which are together called cotrimoxazole. They promote each other’s action and therefore, are generally prescribed together. Folic acid is required by the bacterial cell for DNA synthesis, which is also synthesized in-house. These drugs interfere with synthesis of folic acid and inhibit bacterial multiplication. Example: sulphamethoxazole and trimethoprim (cotrimazole)
Chloramphenicol: It prevents the synthesis of bacterial cell wall and inhibits its multiplication.
Example:chloramphenicol sodium succinate
In a nutshell, following are the treatment steps followed for treating cholera:
1. Rehydration The first objective to treat a person affected by cholera is to hydrate their body. Oral rehydration salts (ORS) can help people hydrate themselves quickly enough. Furthermore, rehydrating the body alone drops the fatality rate to 1%.
2. Intravenous Rehydration Intravenous rehydration is used when a person is severely dehydrated.
3. Antibiotics can be used to reduce the amount of diarrhea caused by the affecting bacteria. However, the antibiotics cannot alone cure you from cholera.
4. Consuming foods or supplements rich in zinc can decrease the duration of diarrhea in children
Read the medication in detail here…
Care:
Following steps can be taken by the care givers of a cholera patient to help him recover soon:
1. Administer frequent ORS solution to the affected individual, after every 15-30 minutes. Your goal is to keep the afflicted hydrated. Maintain intake and output record of body’s fluids, if possible.
2. Wash the bedding and sheets used by the cholera patient with warm or hot water. This will prevent the spread of infection.
3. Try using rubber gloves while cleaning the areas where a cholera patient has defecated.
4. If the condition gets severe, take the patient to a medical care unit without any delay.
5. Ensure proper disposal of patient’s excreta so that others do not get affected.
6. Closely monitor the patient for his hydration state and look out for signs of dehydration, like sunken eyes and wrinkled skin. Patients in the extreme age groups, i.e. above 75 years and below 3 years, should be monitored meticulously.
7. Look for weak pulse as it might indicate a life-threatening emergency.
8. Try to keep the patient in the sitting positing, especially in the beginning of rehydration therapy, as it can help in keeping the patient alert and improve oral tolerance.
9. Zinc supplements can be started with the onset of symptoms in children as it can help in decreasing the duration of disease.
OTC Medications and Self-Management Methods Available for Cholera
OTC Medications:
No OTC medication is recommended for treating the symptoms of cholera except ORS. If cholera is suspected, ORS should be started immediately, even before confirmatory test results are back. Medical help should be sought as soon as possible, if the symptoms are severe.
Self-Management Methods for Cholera:
1. Drink plenty of non-alcoholic fluids and ORS solutions to keep yourself hydrated.
2. Drink safe and treated water.
3. ORS should be prepared properly, by pouring the entire content of the packet into 1 L of clean and boiled water. Mix the contents properly and keep it covered at normal temperature.
4. Wash your hands thoroughly with warm water and soap after using the toilet and before meals.
5. Even if you are recovering from Cholera, do not swim for at least two weeks.
6. Do not defecate in a water body.
7. Keep the food covered and eat it while it is hot. Do not consume raw or undercooked food.
8. Wash your clothes, yourself, your children and their diapers away from the water source.
Natural Ways to Cure Cholera
Although rehydration and antibiotic therapies are the major treatment plans for cholera, the symptoms can be managed by some of the below mentioned remedies:
1. Onion
Taking onion with cloves can help in minimizing the symptoms of cholera as they possess antibiotic properties. Also, they help in relieving symptoms of dry mouth, thirst and restlessness in the patients.
2. Cloves
Abdominal discomfort can be managed by taking cloves. Eugenol found in cloves helps in killing the bacteria.
3. Fenugreek Seeds
high mucilage content in fenugreek seeds help in bulking up the stools and reduce the severity of the disease. They help in treating severe diarrheal conditions.
4. Turmeric
taking turmeric in small quantities can help in managing severe diarrhea due to its antibiotic properties. However, it should not be taken in large quantities as that can prove detrimental.
5. Lemon
The anti-bacterial property of lemon helps in managing excessive diarrhea in cholera. Additionally, vitamin C present in the lemon helps in strengthening the immune system so that the body can fight the infection more efficiently.

Health Tip by Experts
Cholera is a disease that spreads by consuming drinks and foods made from water contaminated with the bacterium Vibrio cholerae. Although the disease is rarely seen in developed countries, it is still prevalent in developing and underdeveloped countries. Proper sanitation measures at community level is required to prevent outbreak of cholera. If a person still contracts cholera, rehydration and maintenance of hydration state should be the first priority. Antibiotics can also be given in severe cases. No other medicine should be given to manage diarrhea. If treated properly, cholera can be easily treated.








